Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
2 min read
 Team Pulsara
:
Apr 14, 2021
Team Pulsara
:
Apr 14, 2021

EDITOR'S NOTE: Special thanks to Kinsie Clarkson (Pulsara's Product Marketing Specialist, 2020-2025) for writing today's blog post. You can connect with her on LinkedIn.
__
A Canadian study published prior to the COVID-19 pandemic indicates that community paramedicine programs are improving care and outcomes for patients.
According to researchers Michael J. Nolan, Katherine E. Nolan, and Samir K. Sinha, there is a growing need for a more flexible, sustainable model of care to deliver high-quality healthcare within communities—and in Canada, community paramedics are being recognized as uniquely positioned to deliver exactly that.
As the number of unnecessary 911 calls increases each year by 8% in some Canadian jurisdictions and Canada searches for effective ways to improve healthcare delivery for their aging population, community paramedicine offers the opportunity for a more personalized, community-based approach to patient care.
Community paramedicine programs are a growing trend in EMS and ambulance services across North America. As it became clear that the ED was not always the appropriate destination for every patient, medics noticed a need for flexibility in both treatment and transport protocols. And, as the study states, "Because paramedics initiate care for people in their own homes and communities, these health care professionals are well placed to recognize the unmet needs of the community-dwelling individuals they serve and to act proactively to support efforts to stem unnecessary use of emergency medical services."
Community paramedicine was devised as a way to expand the roles of paramedics to allow them to provide a more personalized form of care that meets the individual needs of each patient—whether or not that's a trip to the emergency room.

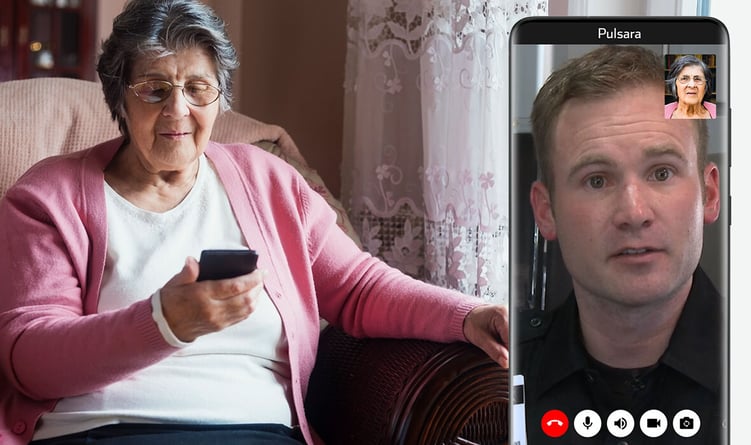
Community paramedics are primarily interested in bridging gaps between service providers and stakeholders. They have the training to offer expanded services to patients in their homes, and can conduct preventive home visits for a number of scenarios: follow-up care after a patient has been discharged from the hospital to ensure they have the resources they need, 911-initiated telemedicine encounters to bring in a doctor to help determine the best course of treatment, treatment-in-place, alternative transport to a healthcare facility other than the ED, and even assistance with chronic disease management for patients in rural areas.
Ultimately, their efforts have been shown to help reduce costs and the number of unnecessary transports. According to the study, "In rural Nova Scotia, a community paramedicine program developed to address a shortage of available primary care services reduced annual trips to emergency departments by 40% and decreased overall annual expenses for health care from $2380 to $1375 per person. In rural Ontario, a community paramedicine program targeted around medically complex high users reduced 911 activation by 24%, emergency department visits by 20%, and admissions to hospital after emergency department visits by 55% one year after implementation."
Though the study was published before the onset of COVID-19, its findings have been consistent with the continued success of community paramedicine programs throughout the duration of the pandemic. In Colorado Springs and Teller County, Colorado, clinical leaders have initiated a community paramedicine program that leverages secure live video interactions to help reduce COVID-19 exposures while allowing both paramedics and physicians to still interact with and determine the best method of treatment for patients.
As Canada looks to the future of patient care, Nolan, Nolan, and Sinha say that healthcare systems will need to "adapt resource allocation to ensure improved patient care and system efficiency." Community paramedicine programs can help provide sustainable, high-quality healthcare, and may save a great deal of time and money while providing patients with the best, most appropriate care for their needs.
Read the full study here.
Looking for ways to expand your community paramedicine program, or considering starting one? Check out how Ute Pass Regional Health Service District is using mobile technology to become one of the most dynamic community paramedicine programs in the U.S.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...