As hospitals and EMS agencies in Colorado Springs, Colorado, watched organizations around the world respond to COVID-19, they began to anticipate what their own response would look like. “We got to watch what happened in Italy and Europe and then subsequently in New York,” said Dr. Matt Angelidis, the co-medical director for the Colorado Springs Fire Department and AMR, and emergency physician for UC Health at Memorial Central, Memorial North, and Pike's Peak Regional Hospital. “We had time to think about, ‘Is there a better answer, or do we have an alternate way that we can take care of these patients and deliver care?’”
 In spite of all the unknowns, there were a few key things they knew they needed to prepare. “We knew we had to improve transport efficiency,” said James McLaughlin, director of community paramedicine at Ute Pass Regional Health Service District. “We knew that utilizing the most expensive form of transport to the most expensive destination every single time was not going to be a viable solution. We also knew we stood the potential of losing a great portion of our workforce to the virus, either through this or through them being quarantined and things of that nature. We wanted to reduce provider risk of exposure, and we also wanted to expand access to care.” With all of those goals in mind, they knew that transporting on every call was not going to be a feasible option.
In spite of all the unknowns, there were a few key things they knew they needed to prepare. “We knew we had to improve transport efficiency,” said James McLaughlin, director of community paramedicine at Ute Pass Regional Health Service District. “We knew that utilizing the most expensive form of transport to the most expensive destination every single time was not going to be a viable solution. We also knew we stood the potential of losing a great portion of our workforce to the virus, either through this or through them being quarantined and things of that nature. We wanted to reduce provider risk of exposure, and we also wanted to expand access to care.” With all of those goals in mind, they knew that transporting on every call was not going to be a feasible option.
About the same time, telehealth restrictions were lifted in response to the pandemic, and its growth exploded as physicians sought a way to stay connected with their patients and continue with regular appointments.
In Colorado Springs, healthcare providers and EMS leaders began thinking outside the box. What if telemedicine could serve a greater purpose, beyond just scheduled appointments? Could telemedicine be moved out of the clinician’s office—and into the back of the ambulance?

They decided to test out the idea, and partnered with Pulsara to make it happen.
When COVID-19 hit, the Ute Pass Regional Health Service District was already using Pulsara to streamline communication between their care teams. As a scalable communication and telehealth solution, Pulsara enables dynamic communication between EMS and hospital staff, allowing them to exchange vital patient information, seek second opinions, and share relevant case information through a HIPAA compliant platform.
Both hospital and EMS providers in Colorado Springs were already comfortable using the platform to communicate with one another, so EMS and hospital leadership decided that it might also work for communicating with patients.
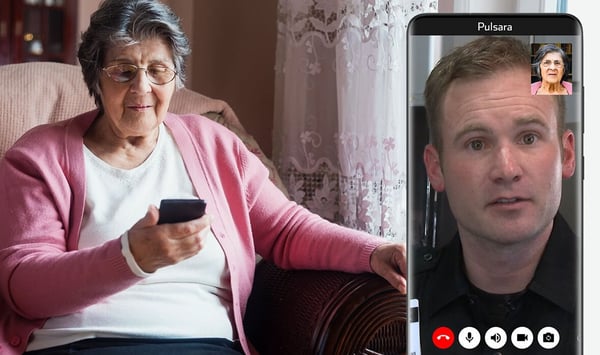
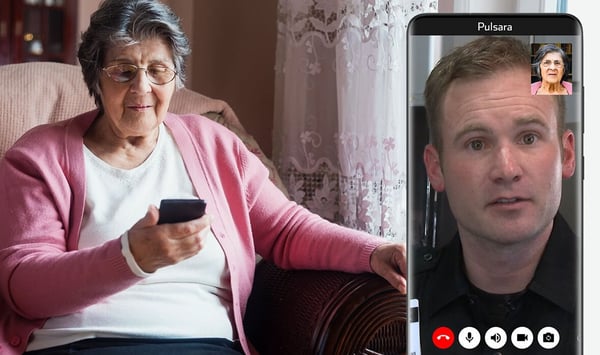
In response to the pandemic, Pulsara released Pulsara PATIENT, a patient-facing telehealth version of the app that enables video communication from providers to patients. Colorado Springs began using the app for telehealth—both in the hospital, and in the ambulance.
Over the past eight months, they’ve learned quite a bit from their experience. They’ve come up with many groundbreaking ways to use telehealth to not only mitigate the risk of exposure to COVID-19, but also use it as a force multiplier and provide patients with the highest possible quality of care.
Last month, Dr. Matt Angelidis and James McLaughlin hosted a presentation to share how their respective organizations are collaborating, communicating, and caring for patients with Pulsara—from the simple, routine patient consultation, to the complex and multilayered COVID-19 pandemic. (View the full webinar below). Here are the top five takeaways from that presentation.
1. One-third of patients that dial 911 don’t actually need emergent intervention, treatment, or transport. Conducting initial consults via telehealth can help quickly determine the best treatment for each patient.
Even before COVID-19 hit the U.S., a significant percentage of 911 calls came from patients that did not need to be transported to the hospital. Not only that, Dr. Angelidis explained, but roughly one in five patients that utilize 911 are repeat callers that have already been evaluated, treated, or taken to an emergency department. “We know that most patients who develop COVID-19 don't require emergency department treatment, 911, or EMS response or transport. But in most systems across the country, when a patient calls 911, that invariably ends with the patient being transported to emergency departments.”

By setting up a telehealth consult with patients from the ambulance, medics can respond to less urgent calls via live video. The medic can see the patient firsthand, speak with them, gather more information about what they’re experiencing, determine from there what the best course of treatment for the patient is, and decide whether they need to be transported. In Colorado Springs, this approach has helped determine the right course of treatment for each patient, allowing medics to respond to each call more effectively.
2. Colorado Springs is using telehealth as a force-multiplier to expand the sphere of power for their EMS teams.
Ute Pass Regional Health Service District faces the challenge of covering a large area with limited resources. When faced with COVID, McLaughlin explained, they needed to get creative: “With our current workforce, we run three ambulances and cover 539 square miles. There was no way we were going to be able to meet the potential demand of COVID without coming up with a unique and interesting way to address it.”
They’ve found that setting up each individual provider inside the ambulance with the ability to conduct calls via telehealth has become an immediate force-multiplier for their resources. McLaughlin explained: “We were able to take these ambulances, split up a crew, and have one crew member run one call, while another crew member runs another call. It becomes a force multiplier for us. We can take one ambulance and double the output of that crew.” When not every call needs 911 response on the scene or transport, empowering medics to start a telehealth consultation to determine the appropriate next steps saves time and resources.
3. Telehealth consultations can help mitigate COVID-19 exposure by helping both medics and patients prepare for EMS’ arrival—and give physicians the ability to conduct a live examination via telehealth.
Thanks to the flexibility of telehealth appointments, Colorado Springs has been able to use them in multiple different ways. Once an ambulance is en route to a call, they can do an initial consult with the patient to help prepare them for the encounter. Giving medics the ability to see and talk to patients before ever setting foot in their homes helps both providers and patients know what to expect.
“Paramedics have the opportunity to instruct the patient to place a mask on themselves, to wash their hands, perhaps to move to a part of the house that they don't typically cohabitate in,” said Dr. Angelidis. “They may be asked to meet them on the front porch or in a garage or a utility room, in a place in the home that hasn't developed a high viral load. We're prepping for the arrival of EMS before they even get there.”
Once at the home, medics use a COVID triage tool to determine whether or not the patient needs to be transported. If their case isn’t serious enough to warrant a hospital visit, telehealth can come to the rescue a second time.

This time, a hospital clinician can be brought in to help evaluate and treat the patient in place. Medics alert a designated physician at the hospital, whose sole responsibility for the day is to take telehealth calls. The physician can then see all of the patient information that the medic loaded into the Pulsara app, and, using live video, work with the medic to diagnose and treat the patient. “I can login to the cell phone and take a look at all the documents that James has uploaded. I can see the patient's vital signs, I can look at the history or present illness and physical exam form that he completed,” Angelidis explained. “James can be physically present performing a physical exam under my direct supervision and observation, so as a team we evaluate the patient, and make sure that I have all the information that I need in order to help make decisions for that patient's care.”
Billing documentation can be completed on the scene and loaded into the patient’s Pulsara channel via HIPAA-compliant photos, creating a smooth process for treating patients remotely.
4. Colorado Springs is already using telehealth for follow-up care in the hospital setting, and they hope to expand it to community paramedicine, urgent care and emergency department follow-up.
After seeing how well telehealth has been working for follow-up care in the hospital setting, EMS leaders in Colorado Springs feel that the next logical step is to expand telehealth into other forms of follow-up care and community paramedicine, in order to create smoother transitions in care.
Transitions in care are often when patients are at the greatest risk of a bad outcome, a return trip to the hospital, and in some cases, even death. “These are the patients that we see every single day that we're taking back to the hospital because there was something lost in that transition in care,” McLaughlin explained. For these patients, incorporating telehealth into a community paramedicine program could be a lifesaver. “We can integrate it so that a community paramedic comes and visits that patient when they're discharged from the hospital. We can power that with a visit and teamed partnership with a telehealth physician, which really increases the power available in that program.”
.png?width=297&name=COVID-19-Goal-3-Limit-Exposure(1).png) To demonstrate, McLaughlin walked through a potential scenario. “Think about a patient who's released for a hip fracture, or a recent stroke. We can come into the house and do a fall risk assessment, because falls are the number one reason that patients bounce back. We're going to make sure that they got the medications that they were supposed to get upon discharge, make sure that they understand how to take those medications, and the risks and benefits associated with those medications. We're also going to make sure that their oxygen was delivered, so that all those aspects are in place and the patient understands their discharge instructions. When a patient is released from the hospital, more often than not all they hear is, ‘Blah blah blah, you get to go home.’ Then they get home and they're faced with this stark new reality that is, ‘I’m home, I'm alone, and I have no one.’ We want to be that someone, we want to be that support so that we can help them make sense of their discharge instructions and be part of the team that empowers them to be successful upon their discharge.”
To demonstrate, McLaughlin walked through a potential scenario. “Think about a patient who's released for a hip fracture, or a recent stroke. We can come into the house and do a fall risk assessment, because falls are the number one reason that patients bounce back. We're going to make sure that they got the medications that they were supposed to get upon discharge, make sure that they understand how to take those medications, and the risks and benefits associated with those medications. We're also going to make sure that their oxygen was delivered, so that all those aspects are in place and the patient understands their discharge instructions. When a patient is released from the hospital, more often than not all they hear is, ‘Blah blah blah, you get to go home.’ Then they get home and they're faced with this stark new reality that is, ‘I’m home, I'm alone, and I have no one.’ We want to be that someone, we want to be that support so that we can help them make sense of their discharge instructions and be part of the team that empowers them to be successful upon their discharge.”
“We also have partnered with skilled nursing facilities and long-term care facilities,” added Dr. Angelidis. “We see this telehealth connection through EMS and community paramedicine as sort of the tip of the iceberg here with regards to expansion. Pulsara is already used in our community, so it's easy to adapt to a telehealth model.”
Before the end of the year, Colorado Springs is hoping to implement Pulsara for direct hospital referral, as well as incorporate the team effort between medics and telehealth physicians as a regular part of their community paramedicine program.
5. From one EMS leader to another: Is your organization ready?
Colorado Springs has seen a great deal of success in their COVID response efforts, and they have plans in place to carry forward their innovative channels of communication into the future.
As they wrapped up discussing their practices, McLaughlin issued a challenge to other EMS leaders to ask the following questions, and take the appropriate steps to prepare for the challenges ahead. “As a leader of your organization—and I believe everybody has an opportunity to be a leader within your organization—I would ask that you ask yourself these questions openly and honestly:
- Is your organization ready?
- Do you know who you're going to need to work with, what equipment you're going to need, and how you're going to get it?
- Have you set the expectations and prepared your workforce?
- Do you understand what your vision is and what your community's needs are?
- Have you set that vision and expectation for your workforce so they know where you're heading? Have you prepared them with the education and training that they need? Have you offered them community paramedic courses?”
Telehealth will remain an integral part of Colorado Springs' patient care far beyond COVID-19.
The COVID-19 pandemic has brought about many challenges for EMS. In the face of hardship, though, Colorado Springs chose to meet the obstacles with innovation. Their goal is not just to treat patients, but to care for each person on an individual level.
The telehealth practices they've been testing over the past 8 months are enabling them to do just that. Looking to the future, these new methods will form the basis of their continued efforts to provide patients with the best, most personalized care possible.

To learn more about how EMS leaders are using Pulsara to respond to the COVID-19 pandemic, check out How Austin-Travis County Uses Pulsara to Manage the COVID-19 Crisis and Beyond.
 Team Pulsara
Team Pulsara

 In spite of all the unknowns, there were a few key things they knew they needed to prepare. “We knew we had to improve transport efficiency,” said James McLaughlin, director of community paramedicine at Ute Pass Regional Health Service District. “We knew that utilizing the most expensive form of transport to the most expensive destination every single time was not going to be a viable solution. We also knew we stood the potential of losing a great portion of our workforce to the virus, either through this or through them being quarantined and things of that nature. We wanted to reduce provider risk of exposure, and we also wanted to expand access to care.” With all of those goals in mind, they knew that transporting on every call was not going to be a feasible option.
In spite of all the unknowns, there were a few key things they knew they needed to prepare. “We knew we had to improve transport efficiency,” said James McLaughlin, director of community paramedicine at Ute Pass Regional Health Service District. “We knew that utilizing the most expensive form of transport to the most expensive destination every single time was not going to be a viable solution. We also knew we stood the potential of losing a great portion of our workforce to the virus, either through this or through them being quarantined and things of that nature. We wanted to reduce provider risk of exposure, and we also wanted to expand access to care.” With all of those goals in mind, they knew that transporting on every call was not going to be a feasible option.


.png?width=297&name=COVID-19-Goal-3-Limit-Exposure(1).png) To demonstrate, McLaughlin walked through a potential scenario. “Think about a patient who's released for a hip fracture, or a recent stroke. We can come into the house and do a fall risk assessment, because falls are the number one reason that patients bounce back. We're going to make sure that they got the medications that they were supposed to get upon discharge, make sure that they understand how to take those medications, and the risks and benefits associated with those medications. We're also going to make sure that their oxygen was delivered, so that all those aspects are in place and the patient understands their discharge instructions. When a patient is released from the hospital, more often than not all they hear is, ‘Blah blah blah, you get to go home.’ Then they get home and they're faced with this stark new reality that is, ‘I’m home, I'm alone, and I have no one.’ We want to be that someone, we want to be that support so that we can help them make sense of their discharge instructions and be part of the team that empowers them to be successful upon their discharge.”
To demonstrate, McLaughlin walked through a potential scenario. “Think about a patient who's released for a hip fracture, or a recent stroke. We can come into the house and do a fall risk assessment, because falls are the number one reason that patients bounce back. We're going to make sure that they got the medications that they were supposed to get upon discharge, make sure that they understand how to take those medications, and the risks and benefits associated with those medications. We're also going to make sure that their oxygen was delivered, so that all those aspects are in place and the patient understands their discharge instructions. When a patient is released from the hospital, more often than not all they hear is, ‘Blah blah blah, you get to go home.’ Then they get home and they're faced with this stark new reality that is, ‘I’m home, I'm alone, and I have no one.’ We want to be that someone, we want to be that support so that we can help them make sense of their discharge instructions and be part of the team that empowers them to be successful upon their discharge.”![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)

