Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...
5 min read
 James Woodson, MD
:
Jul 26, 2021
James Woodson, MD
:
Jul 26, 2021

Editor's Note: The following post is adapted from a presentation Dr. James Woodson recently gave at the Arab Health Conference in Dubai on June 24th, 2021 entitled "Enabling Networked Communication: How Innovations in Mobile Technology Can Be Leveraged For Better Quality Of Care." Though the content was specifically tailored for conference attendees, the principles Dr. Woodson shares apply to healthcare systems worldwide. (Watch the full presentation below or at this link, and check out Part 2 and Part 3 of our blog coverage.)
As a board-certified emergency physician, I practiced medicine for many years in several different areas of the United States. Through my clinical experience, I discovered that my passion was actually to focus on systems of care: How do you combine multiple different organizations, resources, and people together to quickly surround a patient and provide care for them?
For the past decade, I've been studying how to leverage mobile technology to be able to bring people together, and how to actually create a shared consciousness around a single patient event.
Digital health is a massive, multi-faceted landscape. The current emphasis on chronic care management, health, and wellness is incredibly important—and as healthcare begins to decentralize, that's where the focus should be. However, my focus is on the acute care space and uniting care teams.
The acute care space usually serves patients that are often undifferentiated and have an unscheduled and unstructured need. When an event happens, how do they enter into the acute care system? How do we get the right patient to the right facility with the right resources at the right time?
Heart attack, stroke, trauma, sepsis, and cardiac arrest are some of the leading time-sensitive emergencies. These types of emergencies are low volume, but are very high impact encounters, considering the morbidity and mortality associated with these events. This is, when you think about, the last opportunity to provide preventative care.
But in order to provide care for these patients, we need to successfully coordinate the distributed care teams. Physical distance is part of the package in coordinating care, especially when we're dealing with teams across healthcare organizations: EMS or ambulance, the receiving hospital, nursing homes, referral facilities, tertiary care facilities, or the receiving hubs. During transitions of care, how do we hand off patients from one organization to another, especially for events that need to transit several organizations during the process?
Many clinicians feel the pressure of these problems. We are surrounded by technology, but at the end of the day, we often feel lost. We don't know where these patients are, where they're coming from, or what exactly happened. Data is not available in the EHR.
The next step, then, is to discover what needs to be done in order to collect all the data in one place and simplify communication across all the care teams.
The first place to start is examining team cognition.
In the simplest terms, team cognition is how we think as a collective. It's how data, information, and knowledge important to the functioning of a team is organized, represented, and distributed within that team.
When you talk to CIOs across the world, they feel like when they implemented all these EHRs, they were so focused on data and data management that they lost sight of some of the key things that need to be done. One of these is team cognition. But just because the data may be in an EHR, a specific data repository, or a dashboard, it doesn't necessarily mean the information will be accessible. If it's not presented in the right way, it can be almost useless to us.
The environment of acute care is often much different from chronic care. Unlike chronic care management, acute care patients are unstable, they're often in transition, and they're undifferentiated. They just know that something is wrong—something's hurting, something's off. More importantly, they're not scheduled. Many of the providers who care for them are mobile. Those are the providers we're trying to unite and gather a team around.
When looking at the process, we sometimes fall prey to the notion that if we just get the information to the emergency department, we're done. Well, what about all the providers that are going to be taking care of the patient? They're in chaotic environments. They're mobile. And often, you don't know which providers are needed. How do you tag that right person so that they know they need to respond?
The teams that we're trying to mobilize are often very rigid in function and struggle with situational awareness around a specific event. Many times there are middlemen trying to facilitate, but they're playing the telephone game. Similar to the data problem, a lot of the technologies they use to communicate are not interoperable. If you look at how we unite organizations today in healthcare, it's still fax, phone, and radio for the real-time communication exchanges in which we say, "Hey, I've got something that needs to move." The data often is in silos. And even when that information is available, it may be missing context. Not to mention, a lot of the data and technologies are based on proprietary systems.
The companies listed below are platform-based businesses that connect people with similar needs and interests across great distances.
One of the central components of all of these companies is communication. Yet how many of these platforms leverage fax, phone, and radio to accomplish their customer-facing interactions and processes?
The answer, of course, is none. But when you look at the healthcare system and examine a traditional patient journey, all of these red lines (pictured below) are basically communication fragments. They are communication channels that open and close, open and close. We are literally playing the old-school telephone game.
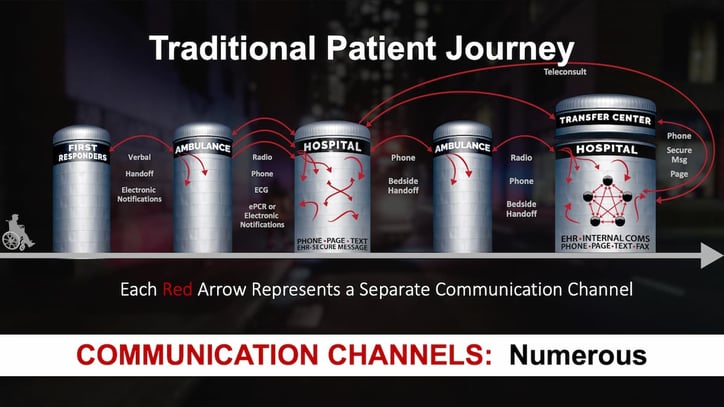
So, a medic may send some information by ePCR, another ECG transmission. Then they pick up the phone and call report to someone who never takes care of the patient to let them know what's coming in. Even if the information is transmitted digitally, it's often not pushed directly to the right care team members—especially if there are downstream care team members that need to be there.
There are some successful methods for connecting intrafacility systems, marked by the star in the diagram. These are fantastic systems that help create a shared consciousness. But some of them struggle around team communication, and all of them are relegated to within one silo and one organization. None of them connect all providers together. The platforms previously pictured connect buyers and sellers from around the world, logistics organizations, and financial institutions, all with a couple of taps. They never leverage communication in logistics like we do here.
A similar problem occurs when you look at devices out in the field that generate data. You might have some monitors that have their own dashboards, and then ePCRs that have their own dashboards. And so already at that point, where do the providers at the hospital go if they want to see real-time streaming data, especially in the context of a patient that hasn't even arrived yet?
How can you aggregate all the data into one location for a very specific context, for a specific job?
Miscommunication in healthcare is an issue around the world. While the following data is from the United States, every country has its own data. It's difficult to find these stats, because these are things that people don't like to talk about.
Research suggests that medical errors and miscommunication are the third leading cause of death in the United States. A quarter of a million to 400,000 people per year die from miscommunication, with 10 serious complications every single day. These errors affect one in every five Americans.
The fascinating thing about this is that 80% of errors and miscommunications occur during transitions of care.
We need to pause, examine this fact, and reflect on what we can do better to serve our patients in these scenarios and events.
And there are many other costs of ineffective communication:
If most solutions for communicating patient data only cover part of the process, is there a way to connect all care teams on one single patient channel? (Hint: The answer is yes, and that’s what Pulsara is all about. Stay tuned for Part 2 for more discussion, or check out the full presentation here.)
![]()
Over the last few years, a group of leading clinicians in Victoria, Australia have transformed their team communication with cutting-edge technology, successfully reducing treatment times, building relationships between their care teams, and improving patient care. This is their story.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...