Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...
5 min read
 James Woodson, MD
:
Aug 11, 2021
James Woodson, MD
:
Aug 11, 2021

Editor's Note: The following post is adapted from a presentation Dr. James Woodson recently gave at the Arab Health Conference in Dubai on June 24th, 2021 entitled "Enabling Networked Communication: How Innovations in Mobile Technology Can Be Leveraged For Better Quality Of Care." Though the content was specifically tailored for conference attendees, the principles Dr. Woodson shares apply to healthcare systems worldwide. (Watch the full presentation here, or check out Part 1 and Part 3 of our blog coverage.)
Poor communication in healthcare is an ongoing issue around the world. Miscommunication costs over $1.7 billion in the U.S. alone each year, causes 80% of serious medical errors during transitions of care, and contributes greatly to preventable deaths.
When we look for the root cause of the problem, it's actually pretty simple: disconnected human work.
There's a brand new industry on the rise that revolves around the concept of the connected worker. Connected worker platforms started in manufacturing, and are starting to move into other industries. The basic idea behind them is to use a combination of hardware, network, and software tools to enable frontline workers to communicate with supervisors or fellow employees who are in another location.
I think there is a lot that healthcare can learn from these types of platforms. We should be looking at the concept of the connected provider: a healthcare provider who navigates their environment and communicates with other team members through connective technologies. Mobile technology can enable clinicians to ask questions and share information with the right team member at the right time, empowering them to act on behalf of each individual patient within their broader system.
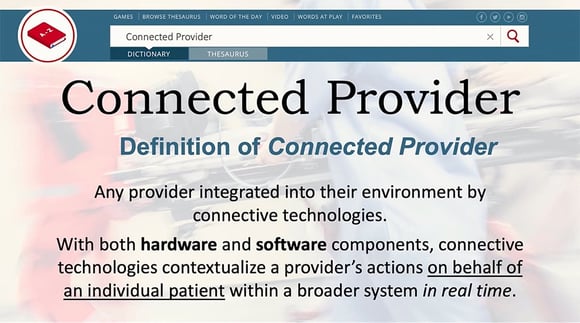
But in order to create this type of system, we'll need to create a system that leverages the right hardware and software components.
Technology has caught up to our needs, but so far, many of the systems we use haven't. From a hardware perspective, many systems are web-based, and so in the early stages, a lot of them were basically confined to desktop versions. However, most of our providers are mobile and constantly on the move.
It's also key that these technologies can interrupt workflows. In chronic care environments, it's more acceptable to expect that people will seek out information, such as visiting a post on a website, or seeking out a link to a teleconference meeting. In acute care environments, however, you need to drive that communication to the clinician.
How can you combine technology that we all carry in our pocket, make it secure, make it private, and make it safe so that you can leverage ubiquitous technology to keep everyone united on the same care team?

Additionally, many systems look at data on the macro level, focusing on coordinating the logistics surrounding many patients. There are other systems that are able to do this on the individual patient level. This is what we've been focused on at Pulsara for the last decade: figuring out how we can connect care team members around a single patient event. How can we get the information all the way downstream to all of the care providers that are going to be taking care of this patient—especially for something that's not in my system, and is unscheduled and undifferentiated?
The sweet spot is combining where data intersects with logistics through real-time communication.
Many times in healthcare, we don't focus on choosing the right communication channel to deliver information from one party to another. Almost all communication in healthcare today is done in linear communication channels. They're very fragmented, and there are many of them, from phone calls to pagers to radios to fax machines. Not only are they not connected, but if the chain breaks once, we've negatively affected a patient's outcome—either with a significant delay, or in some cases, mistakes that generate more patient harm.
And so instead of one-to-one or one-to-a-few interactions, at Pulsara, we are building networks around a single dedicated channel for each patient. And because our platform is built to revolve around each individual patient, it doesn't matter what organization you're with; we can find you, we can drop you into this channel, and everyone has access to everyone else, even across organizations. You have access to other providers via live audio, live video, group messaging, images, notes, and multiple other communication modalities.
Imagine a scenario in which every acute care provider has access to everyone else. You touch a button, the phone rings, and you can connect with a specialist on a live video call. If you need to show them the patient, you can. If it's just a consultation between clinicians, that works too. You can even make group video calls between providers from different organizations. With Pulsara, this type of interaction is now possible.

The other thing that we can leverage is asynchronous communication. During this lecture, I think everybody in this room has done asynchronous communication with someone external. Which is great, right? You can multitask. In healthcare, the technologies we currently use don't give us many opportunities for asynchronous communication. Pulsara leverages audio clips, photos, team messaging, and integrations to enable asynchronous communication between clinicians.
When you build these systems, I think it's important to think about, "Well, this all sounds great, but is there anything really valuable out of it? It sounds like a great solution looking for a problem."
Across the industry, wherever we've implemented Pulsara, we've focused on improving patient safety, reducing treatment times, and improved outcomes. One of the largest things that we see is improved efficiency, which means that organizations are able to do more with less. We've proven that it is possible to reduce these treatment times for time-sensitive emergencies. More efficient treatment times contribute to decreasing patients' length of stay in the acute care facility, which also leads to better outcomes. False activations are another great example; if you don't get that ECG to the right provider for something like a heart attack quickly, they may activate the care team, which is very expensive, only to find out they didn't need to go for an emergent angiography. Pulsara has helped many facilities decrease their false activations through improved communication.

While we're interested in improving quality metrics, one of the things that is really foundational to us is improving the experience for both the patient and the provider. As a physician, I contributed to the EHR data for many years. I took care of the patient, and then I would go back and do the documentation later. So not only is the data not available, but the data for timestamps is kind of made up, right? When we go back to document the times, we often guess. You might say, "I think it was 11:05," when actually the event occurred several minutes earlier.
At Pulsara, we focus on not just uniting care teams to improve care for the actual event, but also capturing excellent data. That way, not only do you have data to show for individual cases, but an amazing collection of data across the region you're looking at, whether it's a single city, an entire region, or even a nation. Much of it is captured passively, which is important as well.
You can also provide instant feedback to the care team. Many people don't think about the fact that ambulance, EMS, and emergency physicians do their job, and then they fade into the background as they move on to caring for other patients. However, real-time education and feedback are essential for helping them do their jobs well. If you look at centers of excellence, they provide all of that data back to the entire care team, even across organizations. That shared information helps the system get better. But instead of spending hours aggregating this data, it can actually go back in real time while that case is fresh and close that emotional loop, which has a positive impact on provider health and job satisfaction.
Our studies go back eight years now, and on average, Pulsara reduces treatment times by about 30%. And what we're studying is not simply prehospital notifications or limited to service-line specific stats in the hospital. It is all that, and more—it's single-channel communication across organizations, and every analysis we do shows significant decreases in treatment times by looking at those efficiencies.
If you're looking at building a system of care, what do you need to look for in a technology backbone infrastructure that can scale? Stay tuned for Part 3 for more discussion, or check out the full presentation here.
![]()
To learn more about how hospitals and EMS organizations are using Pulsara to improve communication, reduce treatment times, and mitigate the spread of COVID-19, check out our COVID-19 info page here.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...