Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...
6 min read
 Team Pulsara
:
May 10, 2021
Team Pulsara
:
May 10, 2021

EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, Marianne Meyers, BS, for EMS1 BrandFocus.
EDITOR'S UPDATE: The ET3 program is mentioned throughout the below article. Please note that, as reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
__
We have experienced a great deal of change this past year, much of it in the realm of healthcare – and particularly in EMS. Moving forward, EMS and prehospital providers can expect to see growth in their role and responsibilities, along with a change in their scope of practice. EMS is expanding to include more than simply emergency response and care – which brings both opportunity and challenges to the workforce.
Here are 10 things you need to keep in mind as the scope of out-of-hospital care grows:
Traditionally, EMS providers have focused on delivering emergency care and stabilizing patients for transport to the hospital. This is changing as more EMS responses are directed toward nonemergent cases and community health initiatives.
For example, throughout the pandemic, EMS providers have taken on nontraditional roles to help fill healthcare needs in their communities. In North Carolina, community paramedics have helped run a COVID-19 testing clinic, and in Florida, EMS providers helped vaccinate homebound patients.
After the pandemic subsides, it’s likely that EMS will continue to treat and manage nonemergent patients with services like blood pressure checks and diabetes management. These healthcare services will promote better management of chronic diseases and improve community health overall. This will also help decrease the number of frequent flyers visiting the ED, which will ultimately drive down costs.

The number of individuals reporting symptoms of anxiety and depression has increased significantly since the onset of the pandemic. In late June 2020, 40% of adults reported struggling with mental health or substance abuse.1
In addition, studies have shown that police spend more time dealing with mental health calls than they do on traffic accidents, burglaries and assaults.2 EMS may be called upon to respond to more of these calls so that the police are able to respond to other matters and, more importantly, so that the individuals involved are provided with the care they need.
Education about local mental health resources, de-escalation techniques and access to mental health workers can help prehospital providers better manage these patients.
The number of EMS transports to the hospital decreased during the height of the pandemic, as patients were hesitant to seek emergency services or hospitalization because of the virus. In fact, one study found about a 25% decrease in EMS calls during the early months of the pandemic.3 This meant that while serious conditions may not have received proper care, fewer nonemergent cases were transported to the hospital as well.

Historically, EMS agencies have been reimbursed only for the patients they bring to the hospital – even those who don’t necessarily need a higher level of care. With the implementation of ET3, however, EMS providers now can also be paid for treating patients they don’t transport. This means there’s no lost revenue when EMS treats on scene, decreasing unnecessary transports and ultimately delivering better patient care.
The Emergency Treat, Triage and Transport model was implemented January 1, 2021, with a goal of decreasing the number of unnecessary hospital transports and admissions, saving money and reducing the overall burden on the healthcare system.4 With ET3, EMS providers can be reimbursed by Medicare for treating patients in place or transporting them to appropriate alternate locations, such as a primary care clinic or mental health center.
The ET3 model will help free up EMS providers to respond to true emergencies like STEMIs and strokes, as ambulances won’t be tied up transporting nonemergent patients to the ED. Additionally, the ET3 model won’t penalize EMS agencies for providing appropriate care. Not every patient needs ED evaluation and hospital admission, but under the previous regulations, EMS would not have been reimbursed for patients they assessed and possibly treated on-scene but didn’t transport.
Now with Medicare reimbursement available whether the patient is treated on-scene or transported, EMS providers are better able to determine what treatment or location is best for the patient without worrying about lost revenue.
Several researchers have described the potential for EMS and community paramedics to help fill a growing need for access to social services and community resources by assessing individuals and connecting them to the specific resources they need.
EMS can help address chronic problems such as poor diet or food insecurity by connecting a patient with Meals on Wheels or a food bank, for example. Community paramedics can be deployed to help known chronic patients manage conditions like diabetes and hypertension, keeping them stable in their homes instead of in and out of the ED. These providers are also positioned to address issues like addiction, as in one community paramedicine program in Colorado that distributes naloxone kits to patients and educates them about treatment options.
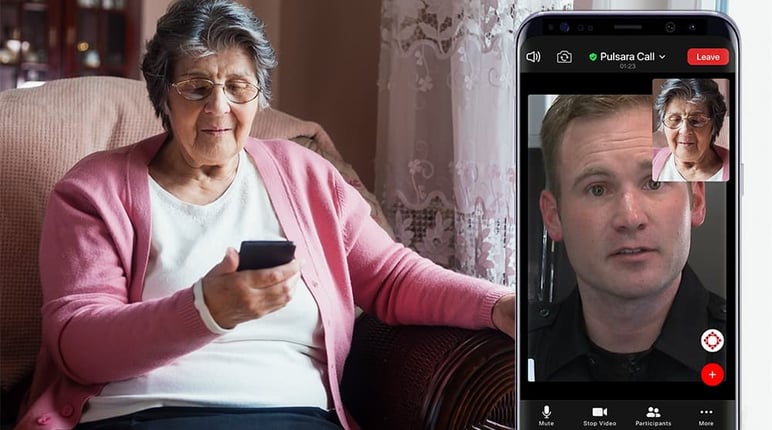
The use of telehealth has exploded this past year, and this trend will continue. Although EMS providers certainly know how to evaluate a patient and treat life-threatening emergencies, having real-time access to a physician or specialist can help with decision-making in the field and ultimately lead to better patient care. Also, the ET3 model requires that a “qualified health professional” oversee treatment in place, and this will continue post-pandemic.
Recently, Congress has passed several bills to help fund telehealth for EMS, so there are opportunities to start using telehealth with your organization. Find out how you can help advocate for increased EMS funding here.
Community paramedicine is often more common with rural EMS agencies serving areas where patients have less local access to healthcare services. As noted previously, community paramedics can help support patients in a variety of ways that complement the patient’s primary care providers. These specially trained EMS providers may be able to help decrease the number of unnecessary 911 calls by keeping up with at-risk patients in the community and providing care that may help prevent them from reaching a point where they need to be hospitalized.
Additionally, EMS providers can and should help educate their communities by offering bystander training on lifesaving techniques such as first aid, CPR, Stop the Bleed, etc. EMS1 columnist Tim Nowak suggests that EMS agencies ought to consider community paramedicine a component of overall community risk reduction. EMS providers can furnish helpful health information – whether focused on providing first aid or managing things like medical alert devices and trip/fall hazard prevention – through a variety of channels, including public training sessions, social media posts and more.
Every patient and community has different needs, and EMS programs should focus on what will make the biggest impact. Deciding as an organization which patient population you want to impact, especially in partnership with a local hospital, will help tailor the medical care you deliver in your community.
Setting out to aid a defined demographic will help your agency measure and demonstrate objectively how your program has made an impact, helping convince local and state legislatures to help fund your program. For example, one California paramedicine program focuses on frequent flyers and those most likely to be readmitted to the hospital. In the first two years, the medics were able to reduce frequent flyer readmission by 50%.
Even though EMS is a critical part of community healthcare, just about every organization struggles with its budget. Community paramedicine can make a big difference in your community, but it’s important to ensure that you will be able to fund it for the long term.

While we are starting to see increased reimbursement from Medicaid and Medicare, this may not cover everything. Contracting with payers and local hospitals is another way to help cover the costs. Community paramedicine has been shown to decrease readmissions and hospitalizations, which saves hospitals a great deal of money. This means it’s in their best interest to help fund programs that will help achieve this.
Through the Hospital Readmissions Reduction Program, Medicare penalizes hospitals for readmission within 30 days for patients with certain diagnoses. Targeting these diagnoses in your community paramedicine program will help show your hospital partners how you are able to save them money, demonstrating your agency’s value and supporting your requests that they help fund your program.
We’ve been taught how to triage during an MCI, but this isn’t a daily occurrence in a typical EMS workday (thank goodness!). Not every patient needs hospitalization, but as noted previously, this has long been the only place where EMS could take patients. Now that regulations are changing, there will be more triaging of patients to determine the most appropriate treatment.
ET3 provides more options for patients and EMS providers, and under this model it’s up to the medics on scene to determine what location would best serve their patients. Familiarizing yourself with the various resources in your community, along with what each can and can’t do, will help you decide what the best option is for each patient – including whether they need transport at all.
The COVID-19 pandemic has changed so many things in healthcare and our society as a whole. The scope of EMS and prehospital care have been expanded faster in the past year than over the past decade, and the industry will continue to change and evolve. Look for the challenges and opportunities unique to your community, as well as the positive changes happening for EMS overall.
About the Author
Marianne Meyers, BS, is a third-year medical student at the University of Washington School of Medicine interested in pursuing emergency medicine. Previously, she was a member of the Santa Clara University collegiate EMS squad where she received her B.S. in Public Health Science. Additionally, she has worked with the King County Public Health Department in Seattle, Washington studying EMT naloxone administration.
![]()
Want to learn more about forming a cutting-edge community paramedicine program? Check out 911-Initiated Telemedicine: How Clinical Leaders Are Using Mobile Technology to learn how leading clinicians in Colorado Springs are pairing innovative technology with community paramedicine.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...