The past two years have done a great deal to redefine the shifting identity of EMS. COVID-19 changed a lot about how we provide care, and some of the solutions we came up with have led to a watershed of self-discovery. With that, though, comes an equal number of questions. What does the shifting landscape of healthcare mean for EMS? What will the role of EMS be going forward? As the identity of EMS evolves and medics are given more agency, will they be able to help find solutions for problems like overcrowded emergency departments, while also giving patients both a better and more appropriate care experience?
Corey Ricketson, Pulsara's Vice President of Strategic Accounts, recently had the opportunity to discuss these and other hot topics in EMS with Chris Cebollero on The Inside EMS podcast, hosted by EMS1. Corey shares his experiences visiting multiple EMS agencies throughout the country, as well as some top takeaways from how leading EMS agencies are finding solutions to issues like ED overcrowding. Chris and Corey talk community paramedicine, how EMS needs to adapt for the future, the importance of meeting patients where they are, and how interoperability, connection, and communication should be a main focus for EMS agencies.
Listen to the podcast below, and read on for part 1 of the full interview!
NOTE: This transcript has been edited for brevity and clarity.
Chris Cebollero:
It is all about going Inside EMS. I am your host, Chris Cebollero. And I am so excited to be with you to end another great week inside EMS. I have a great guest for you, and I am excited to bring him in. Corey Ricketson is the [Vice President of Strategic Accounts] for Pulsara. And we are going to talk about the change in EMS, especially after this pandemic. He's got a great handle on what's going on and some great opinions. Corey, I want to thank you for joining me on The Inside EMS Podcast.
Corey Ricketson:
Thanks for having me, Chris. Appreciate it.
Chris Cebollero:
So I mean, you heard the buildup. When we think about everything that's going on and that's happening inside EMS, EMS doesn't have the same look as it did before this pandemic. I think we've learned a lot of things. I think we've experienced a lot of things, certainly now when we've had our peers pass away because of the pandemic. We've got them living in their cars, or in their mobile homes, or they're just not going home for fear of not transmitting this disease. Then we get a little reprieve, right? We see that things are going to be getting better. And now we're going right back into the same place that we were in before we started. I mean, so from your standpoint, your experience, your expertise in EMS, what do you think the past two years have really done for our career field?
Corey Ricketson:
Well, boy, if we had a crystal ball back in the mid-'90s as to what would've taken place...I mean, it's just astonishing. I got into EMS in the mid-'90s. And in looking back now over the past two years, I'm just seeing a lot of heartache, a lot of challenges, but also, I think a lot of opportunity being presented. We have to look through and find that silver lining and say, "Okay, what are the things that we can take away from this to help propel our profession forward?" And we can sit here and cry over spilled milk and lost revenue, and under-staffing, and all of these different things. I think we have an opportunity to do business in a different way, in a more responsible way, that actually will be better for the public and the customers that we serve.
Chris Cebollero:
You kind of talked about some of the challenges that we have—lost revenue, and all those things. And it seems that in EMS, we're always kind of chasing things. Are we ever really ready for the things that are happening around us? But it seems that we attack them as best that we can, and then our resiliency is really something that really brings us to the forefront of being able to adapt. I mean, so when you think about it from that adaptation standpoint, from that resiliency standpoint, EMS really has a lot of strengths when it comes to dealing with this pandemic. Right? So if we think about where we were in the beginning when we started, and how we adjusted, what do we need to do now to kind of take the next few months by the horns and really kind of wrestle this thing to the ground from a career field standpoint?
Corey Ricketson:
Yeah. I mean, the opportunities are endless. I think we've always been really good in EMS at operating on shoestring budgets and adapting and overcoming. It's what we do. We solve problems each day when we get to a patient's house. And we don't have the same resources as a hospital. And we have to make lemonade out of lemons, per se. So one of the things we have to look at is, "What is our place in the healthcare continuum now?" It is very obvious with how saturated the hospitals are, and the census that's through the roof. We can't get patients transferred, even for minor things that would normally be a no-brainer. "Hey, I've got an appendix that needs to be taken out and I can't do it at this rural hospital. I can't even find a bed to do that."
So we're living in a world now where our resources are taxed. We have an opportunity to step up to the plate as EMS now and say, "We can help. We can help reduce the surge in the first place." We can do the things for some of these patients in an out-of-hospital environment so that we can offer some relief for these nurses and these doctors, and all of the staff that are so taxed in the hospital. Can we do things more responsibly for these patients that are calling and entering the healthcare system? Can we meet them earlier and do the right things for them, solve those problems for them?

I think in every community, that looks a little bit different. Certainly, the resources that you have at your disposal are vastly different in an urban versus a rural area. However, I think that what you can do is look inside your region and say, "What are the problems that need to be solved?" Even if that's starting small and just taking baby steps and starting to understand and learn how to do it, that can evolve into something pretty special over time.
Chris Cebollero:
One of the things you said really kind of brought me to the thought of how community paramedicine fits into dealing with this pandemic. We know that there's a big transition that's going on when it comes to community paramedicine, and you're really kind of making it the forefront of our career field. Then we have to remind people that the first community paramedicine programs popped up in 2007 and 2008. So this is something that's really not new. And you kind of touched on this a little bit in your last response, but how can community paramedics or community paramedicine programs—especially the ones that are established, but the ones that haven't been established yet—how can they really kind of take the step up to say, "Maybe we need to get into this business now"? I mean, we've proven that community paramedics really do well in this space.
Corey Ricketson:
Well, certainly, there's a couple of perspectives there. Number one is: How do you make money doing it? And that's going to differ vastly based on the environment that you're in. But take that aside and say, "How can we do for the public what needs to be done?" I'm sure you were the same way, Chris, but I can tell you that when I was on an ambulance, there were so many patients that I got to and I said, "They don't need a hospital. They just need this." And if I had that as a resource, not only would I get back in service faster and feel better about my job at the end of the day, but this patient would have better satisfaction as well. Nobody wants to go and sit for hours in an ER waiting room to get sutures, or to get a prescription for a medication, or whatever the case is, and then catch some type of infection when they were well when they went in.
But I think that those two things are our priorities. And so if we take the latter and we say, "What are some of the problems that we're looking to solve?" Well, what about if I have a lower acuity patient? And what if I was able to remotely consult a nurse practitioner, or a PA, or even an MD, so that they could have a telehealth consult with my patient while I'm on-scene with them? Would that make a difference and help with secondary triage, being able to potentially remotely prescribe medications, or broker a follow-up visit with a GP, or a specialist, or something like that? Starting at a place like that is pretty simple, and that's where finding the right resources in your community, where you have a doctor, you have an NP, or somebody like that, that's willing to remotely see a patient in these certain situations, where a patient meets inclusion criteria.
Or, we start even earlier than that. This patient enters the healthcare system when they call 911. Well, I've always said, "UPS doesn't send an 18-wheeler to pick up an envelope." Right? I mean, if we know that this is a lower acuity patient, there may be situations where we just don't send an ambulance, but we have relative certainty that this patient's stable enough to go ahead and see a doc, an NP, or even an advanced practice paramedic right now, remotely. That provider can start to understand their problem so that we can put the right solution with that problem. And so meeting that patient where they enter the healthcare system and allowing these folks to do the right thing for them is an important consideration.
Chris Cebollero:
Yeah. And I have to agree with you 100%. I like how you said that [UPS] isn't sending an 18-wheeler. And certainly, we've been taking the most expensive mode of transport, bringing it to the most expensive mode of treatment for long enough. And we've got to be able now to do this. So in your role as [Vice President of Strategic Accounts], you have the opportunity to travel around the United States. You have the opportunity to work with different health systems, work with different EMS systems. Can you talk about some of the best practices that you've seen over the past 18 months to two years, of what people are trying to do to deliver the highest quality of patient care possible, and then keep their employees safe?
Corey Ricketson:
Sure. I think one of the challenges in actually putting this into practice has been public perception. Right? And now we're in a place where the public is asking for this. "I don't want to go to a hospital because I'm nervous that I might catch COVID if I go," or things like that, access. So the appetite is there; from a public standpoint, they're more accepting of this. And we're actually delivering a service that is better for that public perception.

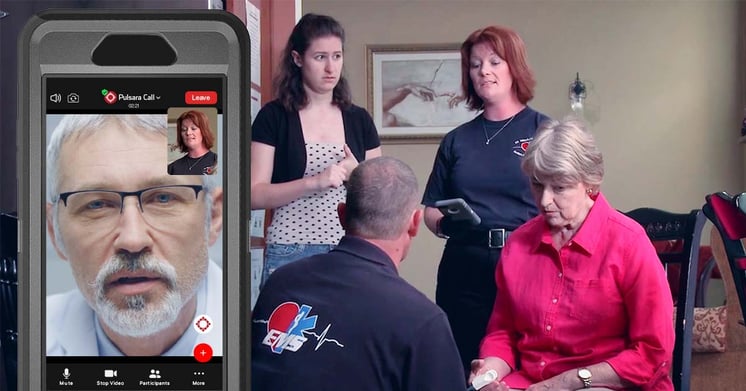
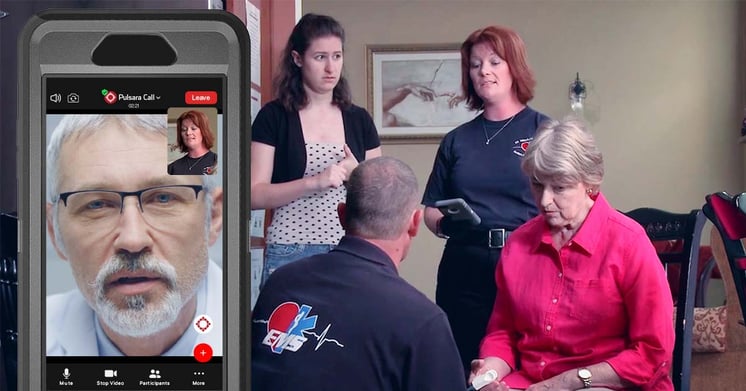
In some of the more astute systems that I've seen, the first thing is, they have a program in place to meet the patient upon that initial 911 call. They have something in place to secondarily triage and put a team on that to be able to further assess the acuity level and what the patient actually needs. Do they need mental health services? Do they need substance abuse services, hospice response, or do they just need lower acuity at-home care? Maybe they need durable medical equipment. They've got relationships that are built now in their community so that they're able to be a middleman, broker those resources, and bring those to the patient.
The second thing that they're doing is giving medics some other potential avenues to take care of those patients. So once I'm on-scene, and we're very good at our jobs, we see thousands of patients over our careers. And we walk in and we say, "Stable, not sick." Do they need a hospital? Yes or no? And if that answer is no, what do they need?
And if I've got a backup, a navigator behind me—I call this concept a "middleman navigation system." We build these hubs in the cloud through our communications platform, where a medic is on-scene, and they say, "I need resources." So they start a channel in Pulsara, and they say, "I'm going to consult in my middleman navigation hub," and that's my problem solver. I've got a team of individuals ready to solve my problem. And they say, "What you got?" And I say, "Got somebody that needs at-home oxygen. They're lower acuity, they are COVID positive. These are the things that are going on."
And then all of a sudden, an MD remotes in, sees the patient, says, "Yes, I agree, and also we should probably throw these medications at them, but let's get some durable medical equipment to their location; let's get these different things." We're keeping the patient out of the hospital. But we're also delivering care that they would expect if they did go to the emergency room while allowing them to stay at home.
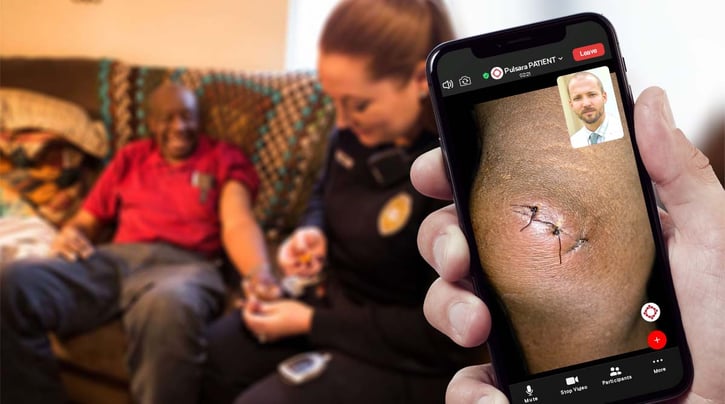
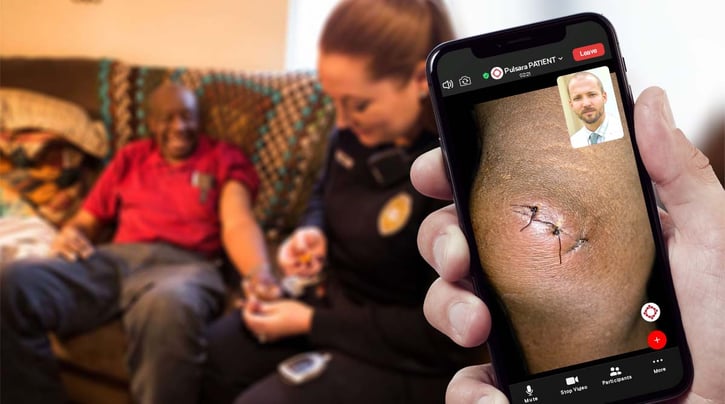
The third thing I would say is that they have follow-up ability. A lot of the reason that we were nervous about leaving patients at home previously is the risk. And it's a very real possibility. But one of the things that we can do is mitigate that risk by saying, "We are going to proactively follow up with you." One of the things that we have at Pulsara is called Pulsara PATIENT. It's a very light app that the patient puts on their phone, and it allows a team to remotely see them through video. It's HIPAA secure, encrypted, et cetera. And so it does allow them to proactively see the patient at the 24-hour mark, the 48-hour mark, whatever that case may be.
We even have programs where maybe they have substance abuse follow-up; so, somebody's going to get medication for that. They can follow up with that patient and say, "Hey, it's time for your next dose. Do you want me to meet you at the Shell station? Because I know you may not want us to come and give you this in your house." Right? So they're just meeting the patients where they are and solving the problems. And it takes that out-of-the-box thinking.
Chris Cebollero:
Yeah. I think that's really interesting. How about for safety? Have you noticed any best practices in the safety realm?
Corey Ricketson:
Well, certainly, we've got one of the programs I helped start in the Austin region early on during COVID. One of the things that they were doing is, on certain types of patients, they would add in either command staff or their decontamination units and things like that. So basically, they were consulted into the channel with the medic and the patient. And then they would respond to the hospital to help decontaminate the unit whenever they arrived. But one of the other things is limiting exposure. You think about the patient safety standpoint: if they don't have to be around other people that are sick, then obviously, they're safer. And limiting the number of personnel that goes to a patient in the first place, that limits the medic's exposure as well.
And so through connectivity and our software, then the platform can actually reduce the amount of exposure that either the patient or the clinicians have. But you still are able to remotely examine them and refer them to the right treatments.
Chris Cebollero:
Right, right, right. No, I think that's a really great point. Let's go ahead and take a quick break, Corey. When we come back, I want to go ahead and talk about emergency management. When we think about this from the standpoint of our business, we had COVID, we've got our regular operations that we've got to deal with. But emergency management is something that we really have to be able to coordinate when it comes to healthcare facilities, when it comes to other agencies, and when it comes to the community. And there's got to be an easy way to do that.
Check out Part 2, in which Corey and Chris will discuss emergency management and better ways to communicate across organizations during a crisis!

With a scalable system of care, Austin-Travis County EMS kept 434 low-acuity patients out of the hospital over just three weeks—and rerouted them to faster, more appropriate care. Here's how they did it.
 Team Pulsara
Team Pulsara



![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)

