Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
Editor's Note: Special thanks to Barry Hickerson, EMT-Pm, for writing today's blog post. Barry is a respected veteran with more than 30 years of experience within the Fire and EMS markets. Currently, Hickerson serves as the Managing Director of marketPOINT, a marketing consulting firm. Prior, he served as Vice President of 5.11 Tactical, a global public safety products company. Prior to joining 5.11, he served as Director of Marketing for Masimo, a worldwide manufacturer of medical monitoring products. He has been an active paramedic and flight paramedic for 40 years, currently serving as a Firefighter-Paramedic in San Joaquin County, California.
—
When I was fresh out of Paramedic school, STEMI and stroke patients were something we couldn’t do much about except monitor and transport. To be honest, we hadn’t even started using the term "STEMI," and we were years away from giving aspirin. Patients who survived to get discharged out of the CCU or ICU (there were no stroke units then) went on to rehab or an extended care facility with a shoebox full of meds. They were armed with lots of Digitalis and Lasix, but not much hope.
I had no idea that, ultimately, we could have some of the greatest impact on STEMI and stroke patient outcomes. tPA, stents, LVO/thrombectomy and specialty teams didn’t exist. We’ve come a long way and, as a caregiver, it’s rewarding to see how emergency medicine has evolved. Especially now that I’m well over 50, stroke and STEMI care have a whole different meaning than when I started my career.
When I started really looking at stroke and STEMI systems, it seemed hospitals and EMS had great plans, good training, and a generally firm understanding that time is the enemy. Unfortunately, I was surprised to learn of the high false activation rates and poor intra-team communications. I witnessed first-hand a family member's journey through a stroke activation in a major receiving center. I was shocked to see the inability of the team to connect and share patient information, and the resulting delays in care. Despite today's greater awareness of the importance of rapid treatment for STEMI and stroke, there remains much room for improvement.
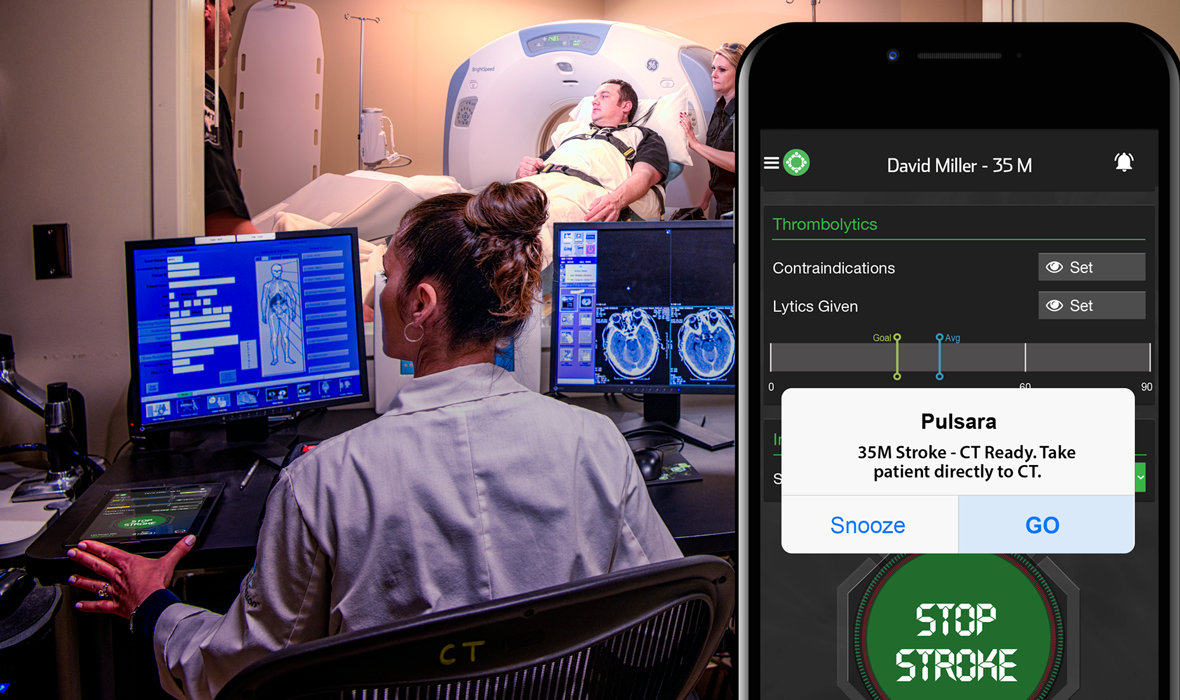
Our understanding of stroke and STEMI has evolved over the years -- why haven't our technologies for managing these cases? Why are we using the same one-dimensional communication systems -- like radios, pagers, and faxes -- that we were using 40 years ago? There’s more transparency and data sharing with my Domino’s pizza delivery than between EMS and the hospital stroke or STEMI team. Without a mobile, real-time, data sharing communication system, teams are poorly informed, decisions and treatments are delayed, and ultimately patient outcome are impacted.
As stakeholders, we should be asking ourselves how we can improve the outcomes of the patients that entrust us with their lives. If a process, product, or technology (like a stroke app or STEMI app) can impact patient outcomes, we owe it to those patients to pursue it. We should never be too busy to seek ways of providing better care.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...