Does Your Team Feel Unseen? Close the Leadership Disconnect with 2-Way Communication
Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
5 min read
 Team Pulsara
:
Dec 20, 2023
Team Pulsara
:
Dec 20, 2023
As 2023 comes to a close, we're pausing to look back at the case studies and research findings published by Pulsara customers. From streamlining emergency response times to enhancing patient outcomes, the stories published this year showcase the transformative power of collaboration, cutting-edge technology, and the relentless pursuit of excellence. Join us as we explore the accomplishments of our customers in 2023, celebrate their stories, and highlight the results they've achieved this year!

National Park Medical Center (NPMC) is a 163-bed hospital that has been delivering care to the community of Hot Springs, Arkansas, for nearly 70 years. Offering a full range of inpatient and outpatient services, NPMC is also home to the Heart and Vascular Center of Central Arkansas, and was recently awarded Chest Pain Center Accreditation with PCI through the American College of Cardiology Accreditation Services.
Previously, when the emergency department received an ambulance call that a patient was experiencing chest pain and possibly a STEMI, an ECG would be sent from the ambulance to the emergency department by fax. But the transmission wasn’t always successful, and even when the ECG did make its way to the ED, there were hiccups in communicating the information to vital members of the healthcare team. According to Emergency Room Director Priscilla Couch, RN, MSN, “Our ER doctor would call the cardiologist and try to explain the patient’s condition without a visual, which takes time. Then, with limited information, the cardiologist would have to decide, well, is that a real STEMI or not?” That deliberation would leave Couch waiting before she put out calls asking cardiac cath lab staff to assemble. “When a patient is experiencing a STEMI, those are precious minutes that are being wasted,” Couch says.
In an effort to improve patient care, National Park Medical Center chose to adopt Pulsara. The instant coordination of care Pulsara provides has helped decrease time-to-treatment for both STEMI and stroke patients at NPMC. The American Heart Association’s guidelines recommend a door-to-balloon time of 90 minutes for best patient outcomes. For the three most recent consecutive quarters, they achieved an average door-to-balloon time of under 60 minutes for STEMI patients. National guidelines call for a door-to-CT time within 25 minutes for suspected stroke patients. National Park Medical Center also decreased their average door-to-CT time for stroke patients from 30 minutes to less than 6 minutes — a remarkable 80% decrease.
To learn more about how National Park Medical Center reimagined their STEMI and stroke communication with Pulsara, view/download the full case study here.
 Communication among interdisciplinary care teams is essential to excellent patient care. Though mobile technology has become more common in various branches of healthcare communication, few have analyzed the process of implementing a tool that works across multiple teams and organizations.
Communication among interdisciplinary care teams is essential to excellent patient care. Though mobile technology has become more common in various branches of healthcare communication, few have analyzed the process of implementing a tool that works across multiple teams and organizations.
The Journal of Evaluation in Clinical Practice published the results of a study designed to determine whether it is feasible to implement a single digital health communication application across multiple healthcare organizations and hospital departments.
Authored by a team of Australian healthcare leaders, researchers, and clinicians, the study includes process analysis from researchers who implemented the Pulsara platform across EMS and hospital teams, as well as written feedback from EMS and hospital clinicians who participated in the implementation. The study explores barriers, factors contributing to a successful implementation, and factors associated with clinicians' intentions to use the technology.
In addition to analyzing the implementation process, the study confirmed that with the use of Pulsara, off‐ambulance stretcher times improved by 8 minutes for patients with suspected stroke and 4 minutes for patients with ST‐elevation myocardial infarction (STEMI). Stroke cases received ED review 17 minutes faster, and CT scans were conducted 44 minutes faster.
The study concluded that "a single communication system can be implemented with good acceptance across multiple healthcare organisations providing prehospital and intra‐hospital care." Supporting the development of habitual use of the app among personnel is essential, as is hands-on training, support for change management, and evidence‐based strategies for shifting behavior. Other critical factors for success include:
To learn more, view/download the full published study here.
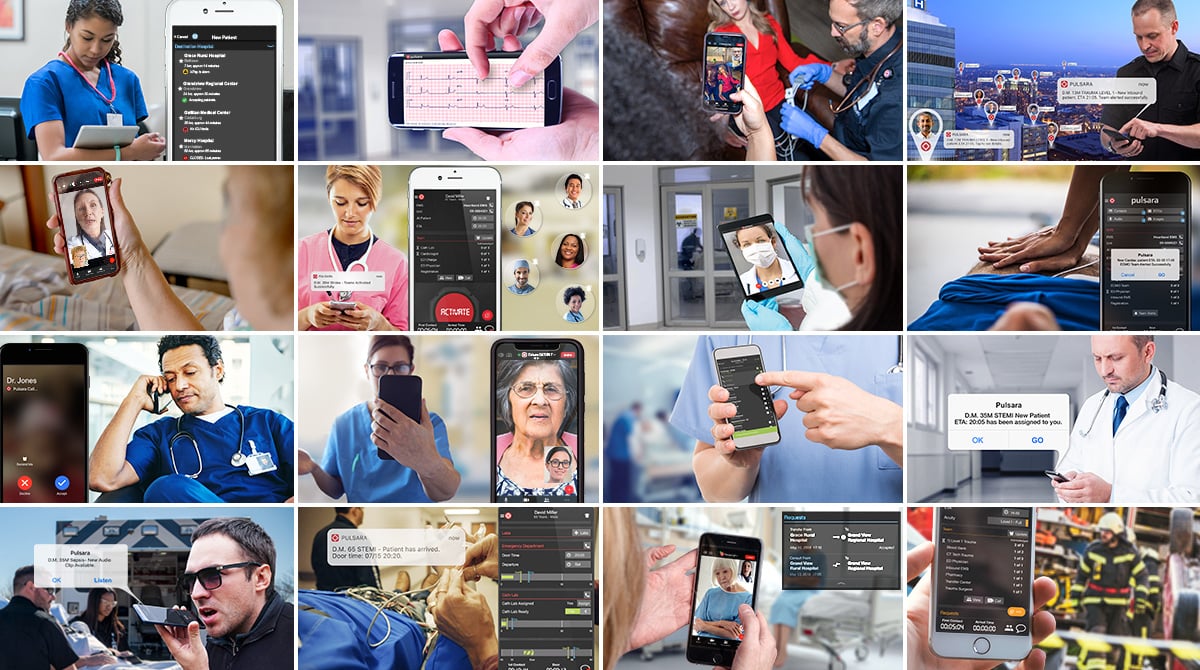
 Baptist Health Medical Center in Little Rock, Arkansas, is an 843-bed medical center and certified Comprehensive Stroke Center. As the largest private not-for-profit hospital in the state of Arkansas, Baptist Health - Little Rock provides comprehensive services using the latest in innovative technology.
Baptist Health Medical Center in Little Rock, Arkansas, is an 843-bed medical center and certified Comprehensive Stroke Center. As the largest private not-for-profit hospital in the state of Arkansas, Baptist Health - Little Rock provides comprehensive services using the latest in innovative technology.
Previously, the stroke team was notified about incoming patients through phone calls and text messages. The operator would use the paging system to activate a code stroke, and then an additional IVR code stroke as needed. Members of the stroke team would receive the page, which contained only the patient’s location, via text or phone call.
Though the system worked on a basic level, Sharon Aureli, RN, BSN, MSN, SCRN, CNOR, RNFA, CNL, and Neuro Program Line Manager at Baptist Health, knew that a more sophisticated communication system could help their teams reduce treatment times. “I always think there’s room for improvement,” she said.
In response to a statewide initiative to improve treatment times for time-sensitive emergencies, Baptist Health Medical Center - Little Rock adopted Pulsara to improve communication around STEMI cases. When Aureli discovered this, she secured approval to begin using Pulsara to communicate about stroke patients as well, making Baptist Health - Little Rock one of the first hospitals in the state of Arkansas to do so.
Instead of delivering a radio report to the hospital, EMS began using Pulsara to start stroke cases in the field. In five months, Baptist Health's stroke team reduced their average door-to-puncture times by 58%.
To learn more about how Baptist Health Medical Center used Pulsara to improve communication around STEMI and stroke cases, view/download the full case study here.
 Earlier this year, the University of Dundee in Dundee, Scotland, became the first facility in Europe to implement Pulsara. The University began using Pulsara to improve patient care and enhance communication around stroke patients, in combination with radiology AI solution Brainomix. According to a recently approved abstract submission to the Scottish Heart & Arterial Disease Risk Prevention (SHARP) released by the University entitled “Addressing Cardiovascular Disease Using a Novel Communication Tool Pulsara: Digital Communication Pathway of Excellence in Scotland,” the implementation of Pulsara has significantly improved patient care in several areas, including improved door-to-CT times and a reduced risk of communication errors.
Earlier this year, the University of Dundee in Dundee, Scotland, became the first facility in Europe to implement Pulsara. The University began using Pulsara to improve patient care and enhance communication around stroke patients, in combination with radiology AI solution Brainomix. According to a recently approved abstract submission to the Scottish Heart & Arterial Disease Risk Prevention (SHARP) released by the University entitled “Addressing Cardiovascular Disease Using a Novel Communication Tool Pulsara: Digital Communication Pathway of Excellence in Scotland,” the implementation of Pulsara has significantly improved patient care in several areas, including improved door-to-CT times and a reduced risk of communication errors.
In coordination with NHS Tayside and Ninewells Hospital, the University of Dundee began using Pulsara and Brainomix on February 14th, 2023, and concluded gathering data for evaluation on September 19th, 2023. "We analysed door to CT times in a sub-cohort of thrombolysis patients,” the abstract reported. “After the implementation of Pulsara, there was a significant improvement in door to CT times (p<0.05). There was a trend towards better outcome at 3 months, however due to a small sample size, more data is required.”
With the Pulsara-Brainomix integration, clinicians can share and receive more detailed stroke patient information along the whole care continuum, enabling faster and more efficient care. The University of Dundee abstract observed that the Pulsara-Brainomix integration enabled “fewer points of contact [which decreased] unnecessary delays” and the “integration with Brainomix [resulted] in improved times to treatment (IV-Lysis, Thrombectomy).”
The abstract concluded that "The implementation of Pulsara significantly improved time to CT for thrombolysis patients” and recognized the platform’s capability beyond stroke care—to any patient event and every method of arrival. “Pulsara, with its dedicated digital pathways for stroke, heart attack, trauma, resuscitation, and many others, has the potential to save brains, hearts, and lives."
To learn more, view/download the full University of Dundee abstract here.
These 2023 stories and case studies are but a few examples among thousands more that demonstrate the incredible work our customers are doing to improve patient care. Their extraordinary passion, dedication, and care are humbling and inspiring—and we're excited for what's ahead in 2024!
To learn more about how EMS, healthcare facilities, and emergency managers around the world are using Pulsara, check out our customer success stories.

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)
Published research shows how using Pulsara, alongside standardized field activation and a focus on stakeholder relationships, improves STEMI care and...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....