Does Your Team Feel Unseen? Close the Leadership Disconnect with 2-Way Communication
Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
6 min read
 Team Pulsara
:
May 05, 2021
Team Pulsara
:
May 05, 2021

EDITOR'S NOTE: Special thanks to Cynthia Bradford Lencioni for writing today's blog post. You can connect with her on LinkedIn.
__
Imagine that you are a paramedic in a rural region who has been summoned by 999 dispatch to the scene of a home accident. All you know is that there is a patient with suspected burns who is counting on you to save his life. When you arrive on scene, you quickly determine that your patient is a young child of about eight years of age with third-degree burns on at least 20% of his body, including his upper torso and head. He is deteriorating rapidly into shock. Given the extent of his injuries, you realize that per protocol, he needs immediate transport to a burn centre. As your partner begins to start an IV, you radio the regional command centre to provide the patient’s status and urgently request critical-care transport via air ambulance. Precious seconds turn into minutes as you stand by waiting for a reply from the command centre with an ETA for the air ambulance team...
Meanwhile, the command centre for your region telephones the neighbouring region’s command centre to request the transport because unfortunately, your region lacks its own helicopter. The command centre for the neighbouring region creates a new patient case in their CAD system and eventually dispatches the helicopter to you. You are unaware of the dispatch, however, until they make another phone call to let your command centre know that the helicopter has been dispatched and your command centre radios you to pass the information along...

At the same time, your region’s command centre makes a telephone call to the burn centre in yet another region to provide all of this information yet again. Lacking another way to communicate in real time, the air ambulance team must make another radio report to the burn centre to establish communication once they initiate patient care and transport. Even after the young patient arrives at the burn centre, additional phone calls and radio reports among the multiple organisations and teams involved in the care are needed to close the communication channels—from ambulance to command centre, from command centre to command centre, command centre to air ambulance, command centre to burn centre, and air ambulance to burn centre. And yet, despite the urgency in an emergency scenario such as this, none of these communication pathways has yet to be open to everyone on the care team, let alone open at the same time as you have been providing care.
As you drive back to your station, you wonder about your patient and whether he made it to the burn centre and what his status is. But that would be yet another phone call or two, and you wish there were a better way for everyone to be on the same page as you prepare for your next run…
* * *
This scenario is, unfortunately, all too familiar to those who provide prehospital critical care. Moreover, everyone responsible for hospital care can also identify with it. From the missed radio report, to the page sent to the wrong team member, to the time spent not knowing whether the cath lab is ready for your patient, most hospitals’ disjointed communication approaches contribute to fragmentation, delays, and breakdowns.
The patching together of traditional, fragmented healthcare communication channels that open and close during a patient event—radios, telephones, pagers, faxes, emails—causes inevitable delays that negatively impact patient care. Look at how many unconnected communication channels there are for a single patient event such as the one illustrated above.
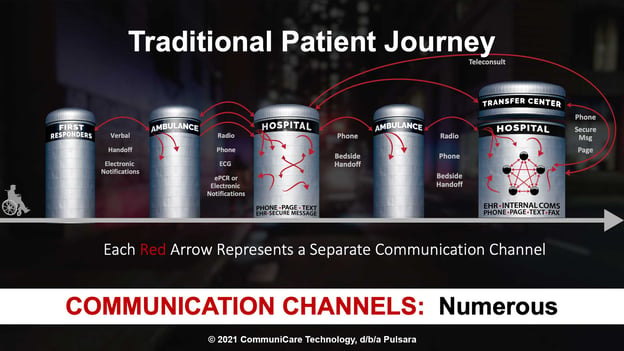
This is a highly inefficient telephone/radio game to play when the stakes could not be any higher. One patient transfer alone can involve numerous—and often redundant—telephone calls, radio reports, and other communications, creating a repetitive, error-prone process where precious time is lost at a time when your most critically ill patients need it the most.
It is very difficult, if not impossible, to create a shared consciousness or unity of effort for critical patient events using traditional communication channels. It is also challenging for care providers to create an accurate clinical picture via radio or telephone—when a photograph of an injury is worth a thousand words.
As an industry, we focus on uniting data, often not in real time with patients’ continuity of care, resulting in fragmented communications that fail to fully leverage modern technology when every second counts. We should be focusing on the team members, logistics, and the communications to actually unite the care teams around the patient’s needs, accelerating lifesaving care.
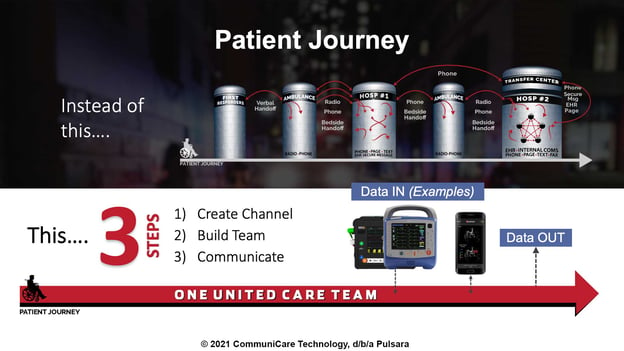
The solution to this problem is networked communication, powered by a rapid, multi-directional flow of information among many-to-many relationships, that is supported by interconnected mobile and online technologies. This can be accomplished by uniting the care team on a single, secure communication channel by means of creating a dedicated channel for a patient event and dynamically building the care team and adding teams, organisations, or individuals on the fly.
Changing circumstances sometimes mean that additional team members, such as a specialist physician or mental-health provider, need to be added to the patient channel for a consult or collaboration. The result is a single source of truth for communication along with shared consciousness via the exchange of synchronous and asynchronous information—data, group messaging, live and recorded audio and video, images, exchange of facility capacity and readiness status, push notifications to all team members indicating alert acknowledgements, and transport ETA based on GPS. Nothing less than these capabilities will be able to unite and create situational awareness and shared consciousness for the entire care team.
In addition, the same networked communication will ensure that all care team members have shared consciousness around the patient's outcome once definitive care is complete at the receiving facility, creating the ability to unify and inform all care teams in real-time as well as the necessary data for quality improvement and quality assurance review. It should be evident that when used to unite the care team across a system of care, a flexible communication and telehealth platform is unsurpassed in facilitating the level of complex care coordination across organisations and geographies that is required to ensure the highest quality of patient care in the shortest amount of time.
By uniting care teams for every patient event, networked communication enables systems of care that scale across time and geography. Whether for a patient case requiring a simple, 1:1 communication or a multi-region, multi-organisation event, such as a mass-casualty incident requiring one-to-many or many-to-many communication, a dynamic, interconnected communication system used each and every day for local, regional, and national stress events is more scalable than traditional communication. The unique ability of such a system to bridge communication and coordination across all organisations participating in patient events, when surge events strain the system’s capacity, reveals its powerful flexibility and scalability.
Siloed teams and linear communication fostering missed information and leading to medical errors is not unique to the United Kingdom, or to any other state, country, or region. The communication crisis in healthcare is a global issue where technology has been a limiting factor until recently. More precisely, it has been the absence of an efficient, unified communication system that has hamstrung clinical teams in even the most high-stakes and critical moments of providing care.
Today, though, leading healthcare systems are creating improved risk and safety profiles by eliminating antiquated, non-integrated communication technologies. Instead of one-to-one, open and closed communication offered by radios, telephones, and pagers, networked mobile communication opens the door to one-to-many and many-to-many communications within patient channels. These channels can be created and used simultaneously and for the duration of the patient event. And in connecting previously siloed teams and organisations—in real time—networked communication supports faster, better coordination and the otherwise more difficult load balancing of available healthcare, transportation, and other emergency resources across Public Safety, Ambulance, Hospital, and Affiliated Healthcare teams within the system. Time to treatment can be optimised and communication errors minimised, with the attendant quality and cost improvements that are demonstrated in the literature.


Systems of care that scale work for any patient method of arrival to the A&E (ambulance, walk-in, or inpatient) and for all time-sensitive emergencies. Any organisation, team, or individual can participate in a patient channel for communication that will enhance intra- and inter-organisational team communications. It is the resultant network, combined with the flexibility of the system, that allows the network to scale beyond routine interactions to enable all of the interactions and communication needed during a stress event. Enhanced communication has been proven to improve the time to assessment, transport, and treatment for critically ill patients.
We can do more to help our healthcare providers to better prepare for the patient’s arrival by improving their visibility into the patient’s condition in the field. We can do more to facilitate the ability of facility staff and remote providers to collaborate on decisions about what care is needed and to determine whether and to which facility a patient’s transfer is most appropriate. We can do more to help healthcare teams to reduce medical errors and delays by reducing miscommunication. We can do more to provide opportunities for feedback that improve care.
* * *
. . . Although you won’t learn of it, you would have wanted to know that your young burn patient has been rather lucky. Despite the many communication handoffs and care-coordination challenges experienced in your siloed system during his care, he has arrived at the burn centre alive and they have been able to make a difference in his outcome. He will forever remember the man in the green uniform with the radio who saved his life. . . .
* * *

The time is now for change in system planning, performance, and delivery to take a new view of leveraging mobile communications technology to unite distributed healthcare teams. In doing so, we will elevate the timeliness and quality of care for those in most desperate need of the best coordinated care, when seconds count. Higher quality at a lower cost will undoubtedly bring more value to any healthcare system that endeavours to make the best use of limited resources and achieve the Quadruple Aim. The time is now.
![]()

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)
Published research shows how using Pulsara, alongside standardized field activation and a focus on stakeholder relationships, improves STEMI care and...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....