In the News: Pulsara's Impact From Preparedness to Lifesaving Care
At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...
3 min read
 Team Pulsara
:
Apr 03, 2019
Team Pulsara
:
Apr 03, 2019

EDITOR'S NOTE: Special thanks to our guest blogger, Lee Varner, MSEMS, EMT-P, CPPS. Lee is the Director of the Center for Patient Safety, and has over 20 years of experience in transformational leadership and patient safety to provide consultation and educational services for improving performance effectiveness, quality initiatives, healthcare best practices, just culture training and patient safety strategies.
__
In your organization, are you proactive or reactive about clinical errors? Isn’t time you develop a plan to reduce preventable patient harm?
It’s been roughly 20 years since the Institute of Medicine published the report “To Err is Human,” which identified that our nation’s healthcare system was harming patients. It’s also been about 7 years since the release of the National EMS Culture of Safety report which discussed similar concerns with EMS (Emergency Medical Services). While there are many differences between the 2 reports, and the clinical settings between EMS and hospitals, there are also many commonalities and parallels between both.
One of those commonalties is the realization that harm reaches patients every day. There are many reasons why harm happens, but one constant is that we are human and prone to error, so mistakes will happen. In addition, most clinical errors are linked to process or system failures. Therefore, it’s not a question of IF harm will reach a patient at your agency, but rather WHEN will it happen, and how bad will the outcome be?
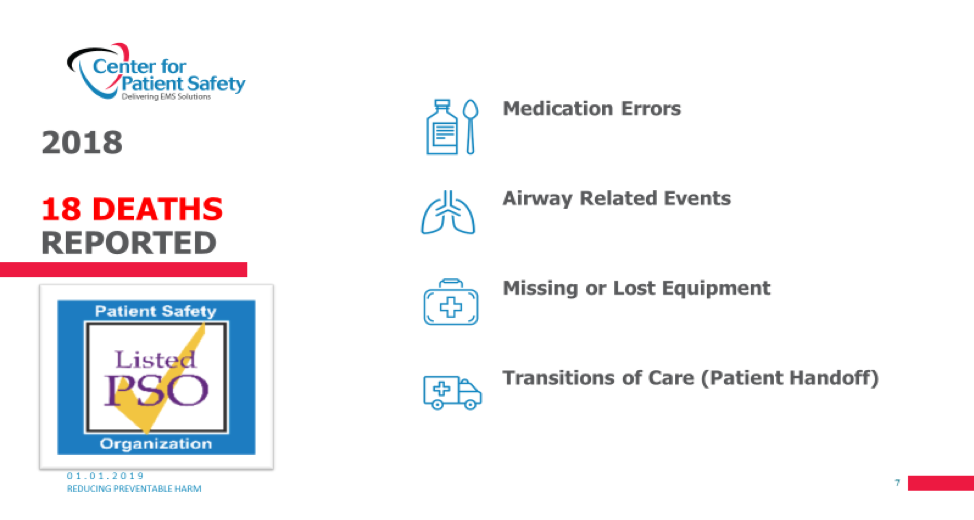
Patient harm happens every day, whether it’s in a hospital, physician’s office or in the back of an ambulance. In 2018, 18 deaths were voluntary reported to the Center for Patient Safety (CPS) PSO, and each of these occurred in the EMS setting. Likewise, each of these events had its own set of causal factors and could be categorized within the 4 areas listed below.
What’s sad is that similar events (most of which are preventable) will continue to happen, and that many patients, families, providers and agencies will be affected. Can every adverse event be prevented? Probably not, but we believe doing nothing and remaining reactive will guarantee few if any improvements. However, becoming proactive will help reduce preventable harm.
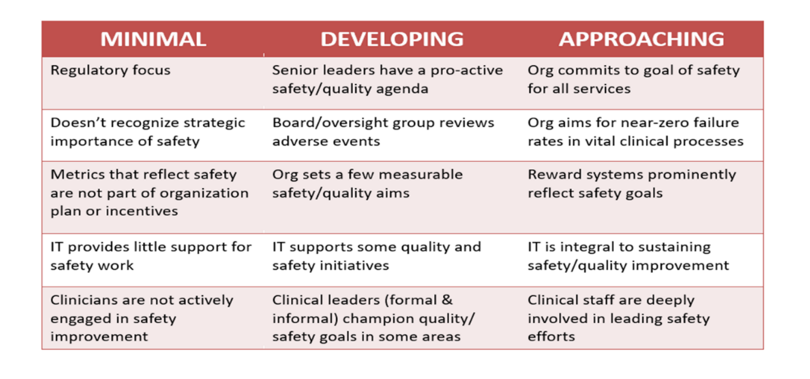
To better illustrate this, the diagram below offers a progression or maturation of safety. It offers a way to think about operationalizing patient safety and some of the important components of a patient safety plan. It also points out some of the cultural barriers that often exist, and which require change from the leadership to the frontline staff.
Over the years, EMS has invested in supporting greater provider and workforce safety. In many cases great progress has been made, however, EMS remains an inherently dangerous occupation. But, the leaders who have taken proactive steps to listen, learn and develop a plan are responsible for affecting change.
In a similar fashion, isn’t it time we made patient safety a value and move from being reactive to proactive with meaningful next steps? While that sounds easy, leaders need to know how to do this work. We recommend they develop an agency plan which will drive next steps and ways to operationalize patient safety, including a means to measure.
EMS, as a profession, is called to change, considering new laws and a healthcare system that is placing more emphasis on patient safety improvements. To meet new expectations and reimbursement models, the advancement of safety in EMS must be a focal point of leadership across the nation. This means shifting from a reactive or unmindful phase about clinical patient harm to a proactive culture based on resiliency and reliability for the patient.
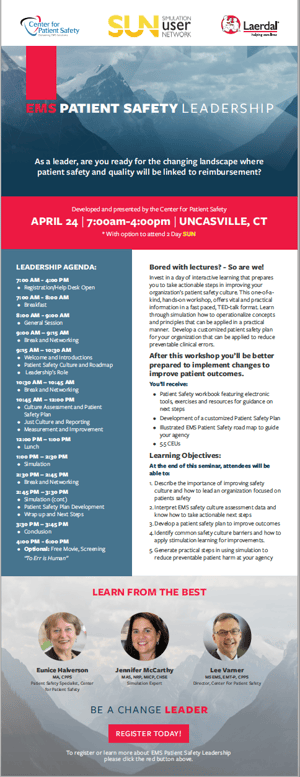 CPS acknowledges the continuous focus on safer care across the continuum of healthcare. To support year-round efforts of healthcare providers, professionals, consumers and payers, we are announcing the EMS Patient Safety Leadership Program. CPS and Laerdal Medical are working in collaboration to support this changing landscape with this new workshop.
CPS acknowledges the continuous focus on safer care across the continuum of healthcare. To support year-round efforts of healthcare providers, professionals, consumers and payers, we are announcing the EMS Patient Safety Leadership Program. CPS and Laerdal Medical are working in collaboration to support this changing landscape with this new workshop.
During the workshop, participants will learn how to interpret safety culture data and take actionable next steps for improvement. They will also learn how to lead an organization that has a focus on patient safety culture as well as how to remove barriers through simulation training. The program will include practical steps to reduce preventable patient harm with simulation and development of patient safety plan for the agency.
The program will be held in conjunction with the Laerdal SUN (Simulation User Network) APRIL 24 at the Mohegan SUN in Uncasville, CT. Join us in learning how to be proactive about reducing preventable harm.
Learn more about the EMS Leadership Program
About Center for Patient Safety:
The Center for Patient Safety is committed to improving safety for both patients and providers. A national not-for-profit organization, CPS serves both EMS and hospitals with a mission to reduce preventable harm.. Its latest tool for EMS, a Safety Culture Assessment, provides agencies with an opportunity to benchmark and improve. Find the Center on Facebook and Twitter @PtSafetyExpert.

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...

December Recap After an incredibly busy events year with 102 conferences, trade shows, and sponsorships, December was on the slower side for us, with...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....