Change is hard for everyone. It's difficult enough to enact across a single organization. So what do you do when change is not only necessary but needed across your entire region?
These are questions that healthcare leaders from Colorado Springs, Colorado, and Des Moines, Iowa, have recently grappled with. The Colorado Springs and Des Moines regions have a striking number of similarities. Both serve a population of around 700,000, have three health systems, and account for around forty EMS agencies. Both have also revolutionized their regional communication with Pulsara, which has allowed them to enable faster, better communication for their healthcare providers.
Leaders from both regions recently hosted a webinar to share their challenges and successes in bringing a new communication system into their region, and what they learned in the process. In part 1 of our blog coverage, we reviewed six takeaways based on their experience. Watch the full webinar below, and check out these six additional takeaways for anyone considering how to approach change management across a region.
1. Socializing change is vital.
While changing the existing system may prove incredibly beneficial, that doesn't mean it will be immediately apparent to all involved. That's why it's important to socialize change and host discussions with those it will affect. David Edgar, MHA, CCP, NAEMT Board of Directors Region III, CAAS Board of Directors, and Assistant Chief of EMS for the City of West Des Moines, Iowa, and Matthew Angelidis, MD, UCHealth ER Physician, Medical Director UCHealth EMS, Co-Medical Director CSFD/AMR, and Co-Medical Director Plains to Peaks RETAC, described how they approached some of the questions they faced in their respective regions.
Chief David Edgar
"My perception in healthcare is everybody is so busy that sometimes trying to tackle change or doing something is almost off the table because people are just struggling to try to make things operate. And sometimes it's [difficult] to even recognize that something could be so helpful to somebody and change the way they do things, and actually make it more efficient.
The initial change management…there are a lot of people that try to torpedo things when it appears to be more work and it's difficult. When we first implemented, I remember the change management folks from Pulsara coming in and telling us that things are going to be identified as problems that are going to be associated with the system we're building up, when actually, it's identifying issues that have been there all along that are now exposed. And I would say that is 100% true, and still proves true today with some of the areas that we're dealing with."
Dr. Matthew Angelidis
"We absolutely used case demonstrations to help our champions in the healthcare systems and EMS system see the benefit of Pulsara. A common issue with STEMI activations is that at 2:00 in the morning, that involves a whole team waking up, opening some expensive equipment, and dirtying a sterile room in the hospital. Pulsara allows us to limit those false activations. We have real-time connections with the actual interventional cardiologist who's driving that ship, and so we see significant cost reduction and time savings, and we're able to take those cases and show them to the teams and the risk management committees and the quality assurance committees, and get real buy-in from our health care systems and EMS partners."
2. Overcoming resistance is about understanding.
Resistance to change can come in a number of different forms, and there are a number of reasons why people will be resistant to change. In today's climate, many people are overworked and are suffering from burnout. Change is difficult under the best of circumstances—let alone when people are tired.
Here's how Chief Edgar and E. Stein Bronsky, MD, Co-Chief Medical Director, Colorado Springs Fire Department, Co-Chief Medical Director, El Paso County, CO American Medical Response (AMR), and Medical Director, El Paso-Teller County 911 Authority, overcame and navigated some of the challenges they faced, and how they got people to buy into their vision for better communication.
Chief David Edgar
"[Something] we've run into from an EMS standpoint is this thought process that, “is this making my job easier, or making the hospital’s job easier?” I've had a couple of conversations with different agencies that are looking at Pulsara, and I think they're looking at it wrong. This is about patient care. I know that's kind of cliche, but we saw it from an EMS standpoint almost immediately when we implemented it, when instead of going to a room and waiting for a nurse, we were going straight to CT on a stroke alert. It really should be about, "this is a patient care thing that we all need to do," no matter where we are in that team. Because if it's your family member or friend, you want that [care journey] to happen rapidly and [with] good information. It's having that understanding that it's not just passing on information."
Dr. Stein Bronsky
"This is one of my favorite subjects to talk about within this whole system, so I'll try to condense it. But the resistance to this was monumental in a lot of ways. The resistance came from the hospital side, the emergency department, service lines, EMS agencies. Everybody had an idea of, ‘why do we need to change something?’
Change is always uncomfortable. And on top of that, what we had to do was tell them to try to project and say, 'this is ultimately our goal for streamlining patient care and decreasing communication errors and delays.' But what really happened was that we had to implement Pulsara alongside of the existing systems.
So there was a certain amount of time (and for us, it was way too long) that the EMS agencies and the hospital systems were doing their normal communication, and then on top of that, they were doing Pulsara. And that was to, quote/unquote, ‘make sure that Pulsara is working and that we have all the bugs out and we really establish it before we flip that switch and turn off the regular or historical communication processes,’ which people really like to hang on to.
And so we were actually asking people to double their work. And you talk to a paramedic in the field, they have so much to be doing, and charge nurses have so much to be doing. Telling them that they were going to duplicate their work was almost a hurdle that we couldn't get over. But we were slowly and steadily able to prove this to people and make them understand that this was just temporary, and that we were going to end up with this robust system in the end that was going to be much better for everybody.
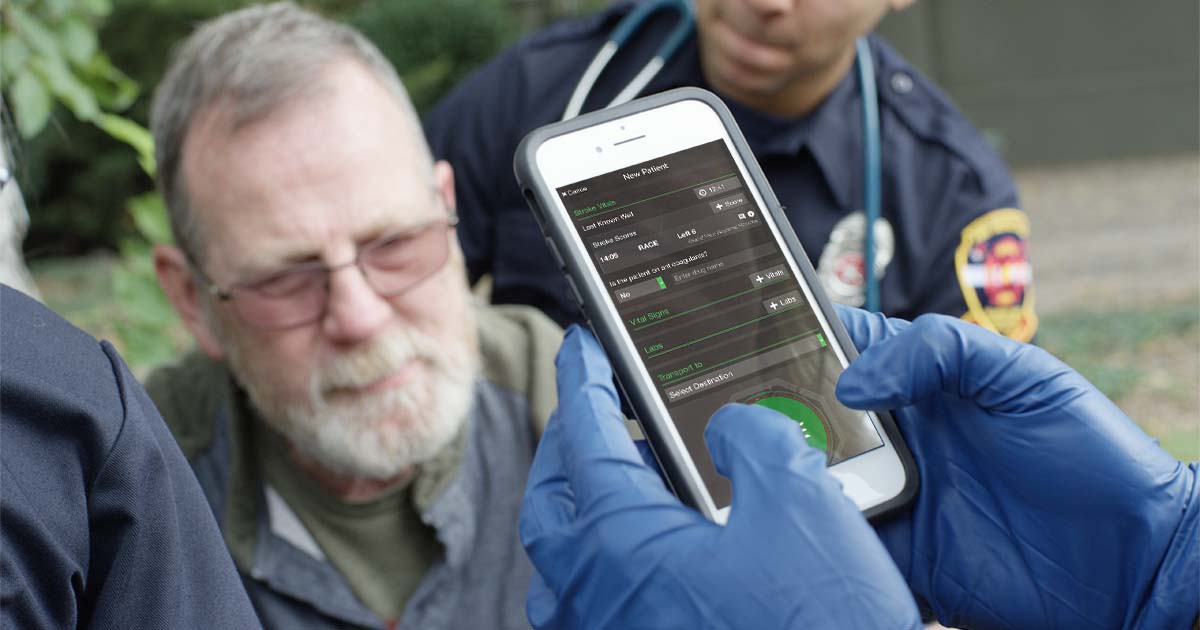
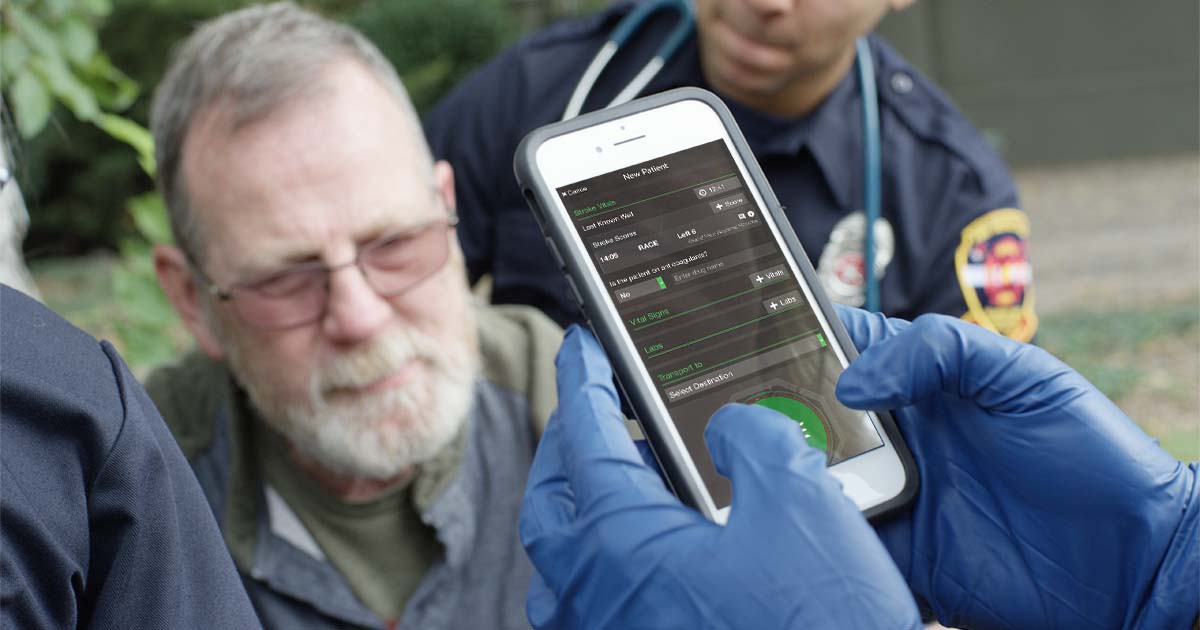
One of the field providers were complaining about the small screens, and the not being able to put in information in the discrete fields, and the charge nurses are complaining about, ‘I can't do everything on a mobile device; I can't keep track of all the ambulances.’ And really, the resolution for all of this was to very consistently show every stakeholder, being in the field or in the hospital, that we wanted to hear what their complaints were, what their issues were.
And then we were able to go back to Pulsara, tell them what our issues were, and Pulsara was extremely responsive to develop a more robust input system and visual system, so that every one of the issues that was brought up from any stakeholder was very rapidly resolved. And it was all resolved according to their feedback. And once they started to understand that that was the process that was happening, people really started to buy into it."
3. Is it better to Push change or attract change? Both have a place in the process.
Change can be implemented in different ways. Change can be "pushed" by being mandated, such as when a region decides to enact a change that everyone has to comply with. But change can also be accomplished by "attracting" people to it—for instance, by communicating with them, helping them understand why you're making the change, and going through that change management process that way. According to Brian Helland, Operations Chief of the Clive, Iowa Fire Department, and Dr. Angelidis, both approaches have a part to play in the process.
Chief Brian Helland
"In the Des Moines area, we did a little bit of both. It depends on knowing your audience. Some of the EMS agencies were on board from the beginning, and it was more of a directive; the push versus the pull. But I think for some of the service lines within the hospitals, it was more of having them see the value.
I remember sitting in a stroke committee meeting at one of the health systems, and the stroke coordinator and the stroke neurologist that was covering for the day were both in this meeting when a stroke alert came over, and we [in EMS] had already been in the process of implementing Pulsara. They had implemented it for STEMI, but not yet for stroke. The overhead page and the pagers went off, and there was a five-minute separation between the stroke coordinator and the stroke neurologist, because that was just one of the communication things.
And it was ironic and kind of funny to be able to say, ‘See, now if you'd had Pulsara, this isn't happening in the STEMI team right now.’ That one instance was a great case, and it sold the stroke neurologist on the importance of getting this change made. So I think it varies based on who your audience is."
Dr. Matthew Angelidis
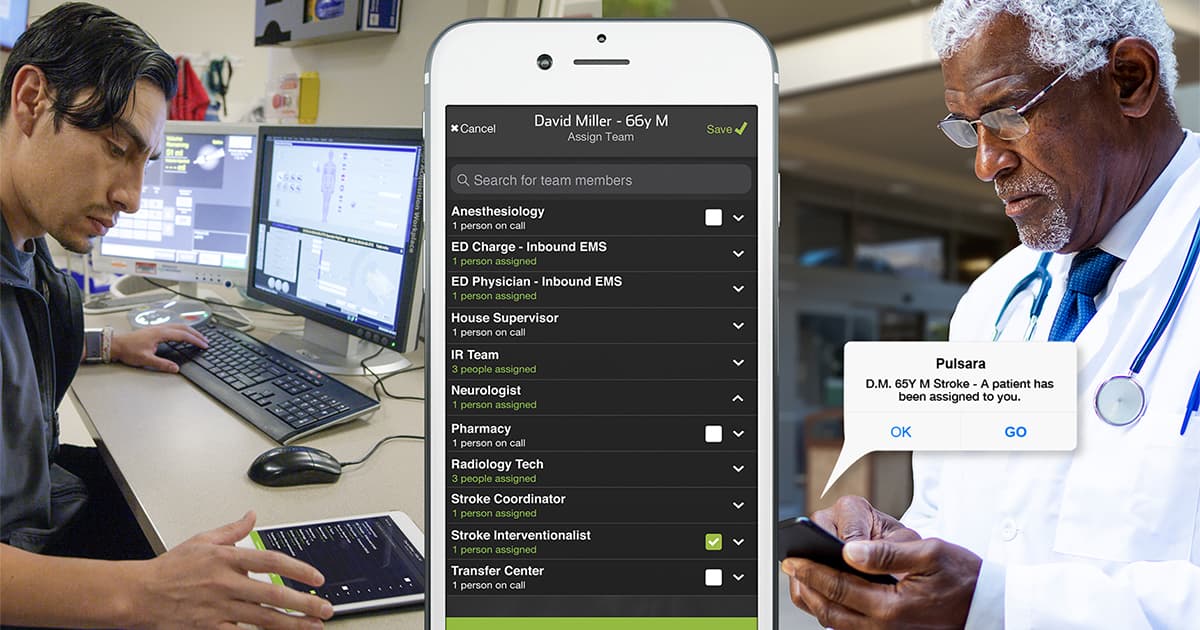
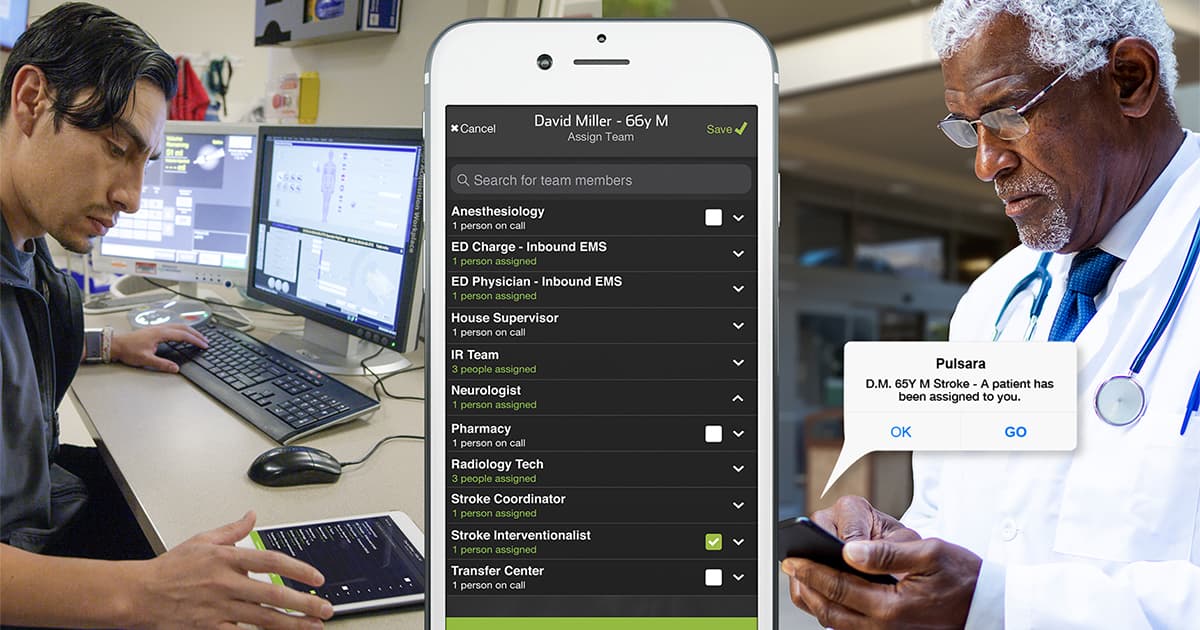
"I think we initiated with a process that I would consider a little bit of a push. But then almost every service line, EMS agency, and health care system that joined the process after that came through the process of attraction. We were demonstrating measurable outcome benefits. And so in our stroke service line, [I] sat in quality assurance meetings with our cardiology service line and showed them solutions to problems that they were having through Pulsara. Then our cardiovascular service line was like, ‘Well, wait a minute, how can we use that? Can you show us that? It works really good for neurology.’ And then trauma followed suit, and now we have a bevy. We have our mental health/behavioral health teams on board. We have our OB/GYN teams on board, we have ICU with cardiac arrest teams.
So as as the system was demonstrating positive outcomes and improvement in communication, everybody sort of starts to see that and wants to know how they can participate."

4. Highlighting wins is important, especially in light of the challenges.
Projects that take extensive change management can be a major challenge. Getting everyone on board and implementing a new system isn't always easy. That's why it's important to celebrate success and highlight the wins when things go well. Here are a couple of the wins that Dr. Bronsky and Chief Helland shared from their regions:
Dr. Stein Bronsky
"I think that the obvious wins are what was mentioned in the last slide. The proof is in the pudding. We can show real measurable improvement in patient care metrics across multiple service lines, and that is a huge win. I mean, you just look at that one fact alone, and the whole thing is worth it. Just for that.
And ultimately, our goals were to decrease communication errors. Which, a lot of people say, ‘Oh, there aren't any communication errors.’ But when you really look into it, there are a tremendous amount of communication errors, and a tremendous amount of communication delays. And sometimes, unfortunately, those can be traced to bad patient outcomes. Not always, but sometimes. And so one of our huge wins was, as we really got everybody on board, and this became the primary form of communication from the field to the hospitals and largely inside the hospitals, up certain service lines—everybody was able to notice right away that the errors in communication and delay in communication just, poof! disappeared. And that alone really brought everybody in. And that's where the attraction comes in as was mentioned previously, that other service lines and other EMS agencies are starting to say, ‘Oh, how can we get in on this?’ And then the other win is really connecting the teams.
That is one thing that was very, very difficult to get across, not only to the hospital systems, but to the EMS agencies—that although they only see their small portion of this, they will begin to realize as we use the system more robustly, that everybody along the designated team is informed, and everybody can communicate, just as Dr. Angelidis mentioned earlier, about how the interventional cardiologists can actually communicate with the EMS crews. How valuable is that? Those are small examples that are just huge wins and successes."
Chief Brian Helland
"Our results in Des Moines echo what Dr. Bronsky just described. It's really a little bit eerie to see how similar the systems are, and the experiences that they had. They implemented their system prior to what we did in Des Moines, and we're seeing identical results in patient care. We've got data that shows that we've decreased our door-to-CT times. We've decreased our door-to-balloon times. And I think David mentioned earlier that we have identified some of those hurdles. People that didn't know we had communication issues, and they were basically identified by using Pulsara."
5. Continuing to nurture the change is vital to maintaining it.
Successful change isn't something where you can just "set it and forget it." Once you achieve your goal, some maintenance and nurturing will be required to continue to grow and develop your program. Here's what Colorado Springs and Des Moines are doing to manage and maintain their regional communication systems:
Dr. Matthew Angelidis
"We talked briefly before about what we call the Healthcare Communications Committee. But we continue to hold bi-monthly meetings with all the stakeholders where we review the cases, we look at what information is coming through Pulsara, and what's missing, and how we can improve it. And then we do education through our EMS systems on interfacing with Pulsara and how to use it more efficiently. And then we created what I'll call a Google Doc—somebody with better IT savvy than me would say it's not that. But essentially an entry point for feedback. So we have the stakeholders all receive emails from EMS crew members, cardiologists, charge nurses, IT providers, a registrar who's registering patients in the ED, you name it. If anybody has an issue with Pulsara, they're able to hop onto a shared web page document and put in their feedback. And we review those every two months at our Healthcare Communication Committee meeting. And then we get really good feedback from you guys at Pulsara.
We can ask for Pulsara reports about volumes, numbers, who's using STEMIs, what features in there are people using, what features should they use. So we get monthly feedback from Pulsara, as well, and we take that back to the Healthcare Communication Committee. I don't see that going away. It's an ongoing, ever-evolving process."
Chief David Edgar
"As Pulsara evolves, there are so many different things to keep people up to date on. Good things, because most of them have come from response from what we have seen in the field on how to improve things. One example of that is we're getting ready in the Des Moines region to remove phone numbers, because that was one of the biggest things if we needed—that phone communication. Now, with Pulsara Calling, it's all device to device. So we're actually going to remove phone numbers and we're thinking that will help take care of one of the biggest frustrations. But you have to keep on it. It's a work in progress. And you always have new people coming in. But it's an important process to keep on top of and pass on.
We can continue to improve. I personally look at Pulsara and the regionalized system as important to healthcare as public access defibrillation. And as far as what it's going to do for—and what it is doing for—healthcare. And if you don't take the time to look at what it is and how it changes healthcare…. That's why I'm a huge advocate, because I see it as hugely important now and in the future to be able to have this communication."
6. Parting advice: Issues are opportunities, and Patience and persistence are key.
When asked to give final advice to leadership in other hospitals and agencies who want to build a regional system of care, the experts had some excellent parting advice.
Dr. Stein Bronsky
"The advice that I would give them is to identify all of the issues they have, many of which they don't recognize, and they have to be prompted to understand that they are issues that have room for improvement. And to show them through data and through experience that Pulsara and this type of communication system can resolve most of those issues right out of the gate. I think that's so important for them to see that correlation and also to understand from a high administrative level that this system really needs to be their ownership. And a lot of times we learned in the past that pushing it through EMS agencies or through one service line was not really the most successful route.
But wrapping in the high-level administrators and showing them the value and then understanding that value, then they take ownership of it and can filter it down through the service lines, and therefore into the field to create these systems of care. And I think that once people understand that, that has tremendous value."
Chief Brian Helland
"I would add in patience and persistence. The changes may not come overnight, and you're still going to have a lot of hurdles. As David mentioned earlier, when we did do the change process, the team from Pulsara came in and identified the fact that there's going to be people that are going to try and torpedo this. And, they're looking for reasons for it to fail. And it's easy to blame Pulsara for the failures, when in reality, the failures were there originally. And Pulsara has the ability to to fix them."
BONUS: Audience Questions and Answers
Q: How would you suggest implementing this program in a city with multiple EMS agencies and hospitals like Seattle, New York City, and L.A.? What's the starting point?
Chief David Edgar
Well, I think there are two different starting points. One is a hospital-initiated starting point, out into the field. And then there's kind of how we did it: EMS-initiated into the hospital setting. But I guess the first thing you have to do is get a group of…. I mean, most places, if they're a larger organization, have some form of—I would hope—some form of groups that meet.
And if you start doing some research and understanding the benefits, you’ve got to get those change agents that are there and understand. I would agree with Brian: leading and doing better is always more difficult than staying the same. To initiate it, you just need to get your key people.
And sometimes, you know, that happens when a system gets stressed, too. So, you know, the pandemic and different things. There are a lot of people that have had to move into better communications and management of people because of the pandemic. So look at those opportunities for improvement and get the proper people and groups educated. It took us probably two or three years to get this established. Now, granted, it was very new at that point, but you’ve got to get people at a table with a common cause first.
Dr. Stein Bronsky
I think that in an ideal world, the best way to implement is to get all of the stakeholders, or as many of the stakeholders as you can, together in the same venue—probably using existing venues that are out there, especially in large cities that have multiple hospital systems and EMS agencies. And really show them the common ground value in this, and really inserting that theory and that idea into the greater system, and not think of it as silos—like, this hospital system, or this hospital system, or that EMS agency. And so that's how I would definitely go about implementing it if I were given a clean slate walking into a community.
Chief David Edgar
One last thing to add is that we finally took money and costs out of the picture. We said, ‘if that wasn't in the picture, does this solve a lot of the problems we were trying to deal with for better information?’ And it was a resounding 100%—everybody there was, ‘Yes.’ Then we worked on the financial issue later. But that can derail you right away, because it’s, as you say, a torpedo. That's an easy torpedo. ‘Well, what's it going to cost?’ And in making the decision with the group on the improvement first and then figuring—in our region, it ended up that foundations ended up fronting the money from the hospitals and other things, and within a week we had the funds to do it, once we made that decision that we were going to move forward.
Kate Leatherby, Moderator
Yeah, I think sometimes it's easier to think of all the ‘why nots’ when faced with large-scale change. It's easier if you're a little bit hesitant and resistant to then just go down the road of, ‘why can't I do this?’ instead of, ‘how can we do this?’ Great points.
Q: Going back to the importance of having a champion for your service line and for your EMS agency, who were some of those people? What were their roles within your organizations?
Dr. Matthew Angelidis
I think in the city of Colorado Springs, our physician medical directors or our EMS agencies were clearly the folks initially aware of Pulsara and bringing it to the attention of our healthcare systems. And then we early on established service line director champions, when Pulsara helped demonstrate to them through some data analysis, ROI for implementing this for our stroke and STEMI patients. So service line leaders within the hospitals.
And then honestly, we had to get our high-level senior administration like CMO, CEO-level folks engaged and on board. Kind of pushing it from the top down, if you will. So we kind of came at it from both angles with champions. But you know, fire chiefs, EMS med directors, service line directors, and then senior administrative folks would be sort of the core group that I would say we kind of worked through and went through to help get it implemented.
Q: How complex of a system is Pulsara? Is it easy to set up and adopt alongside the process of uniting regional health care systems, or is there a big learning curve? Was it easy technology to use, or difficult?
Chief David Edgar
Easy.
Dr. Stein Bronsky
Yes, extremely easy.
Chief David Edgar
I'm not very technical. And I would say especially on the administrative side of it, it is just super simple to use. And most of our folks today use their phones for everything anyway. So it's not a huge jump for them to do that. But no, I think it's a very easy system to use.
Dr. Stein Bronsky
Yeah. And I would echo that. I would say that as long as the background setup has been taken care of (meaning all the IT solutions, everything that needs to be set up for the success of the program), the actual usage from the hospitals and from EMS is really, really easy.
Just to prove a point here, when we launched it in our system, we had multiple EMS agencies that all went live on the same day. And the day that we went live, we recognized that the largest EMS system in our city, which was Colorado Springs Fire Department, hadn't done their training. And we were like 9:00 in the morning, we were going live with it. And so we had to push this training out, and it took people about 5 minutes to figure it out. And so we were actually able to go live with it. Even without Colorado Springs Fire Department having any pre-organized training, the day of. And that is just one point to show just how easy this is.
Dr. Matthew Angelidis
I've personally used it on calls with ride-alongs, and if this old ER doctor can do it, I am very confident our EMS professionals can do it. And they do, quite easily.
Chief David Edgar
I was just going to add, as far as the IT stuff, I've never seen IT stuff get signed off on as quickly with a hospital system as these did. So if you're worried about all these different hurdles, I can tell you that everything is in place for it. That was hospital IT, city IT. It was zero issues on getting that moved forward. And it was quick.
Thanks for checking out our blog coverage of How To Connect Healthcare Teams & Organizations Across Regions. In case you missed it, you can find part 1 here!

For more information on successful change management, check out these 4 Keys For Managing Change Amid Chaos.
 Team Pulsara
Team Pulsara


![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)

