Pulsara Around the World - 2025 Recap and January 2026
December Recap After an incredibly busy events year with 102 conferences, trade shows, and sponsorships, December was on the slower side for us, with...
7 min read
 Team Pulsara
:
Jun 22, 2022
Team Pulsara
:
Jun 22, 2022

2023 UPDATE: As reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Please be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives unaffected by the ET3 program termination.
EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, Cole Zercoe, for EMS1 BrandFocus.
__
Here’s how your agency can use telehealth and community paramedicine to deliver more personalized care to patients
Community paramedicine, mobile integrated healthcare and ET3 are rapidly becoming hot topics in EMS as the profession evolves, especially as the long tail of the COVID-19 pandemic exacerbates issues like ambulance turnaround times.
As ambulance agencies worldwide struggle with long waits at the ED, it’s become even more vital to find solutions to issues like ED overcrowding and long wall times. Community paramedicine, MIH and ET3 possess the unique ability to reduce transports while simultaneously improving care for patients.
Here’s a look at 10 ways EMS agencies can use telehealth and community paramedicine to deliver high-quality care to patients, some of the advantages of implementing such strategies, and how the ET3 model supports this approach.
From longstanding challenges, such as caring for elderly populations, to more recent demands tied to the COVID-19 pandemic, a community paramedicine program is designed to save costs for EMS agencies by diverting non-emergency calls to other health services and by training paramedics to deliver care to low-acuity patients on site.
The reduction in costs can be significant: One pilot program in eastern Massachusetts saved $6 million dollars in one year, or $1,900 per case, and prevented a visit to the ED or hospital admission in 82% of cases. Given the spike in fuel costs this year, one of the most timely examples of how a community paramedicine program and telehealth technology can save agencies money is by helping reduce unnecessary transport costs.
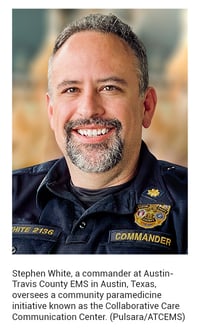
The pandemic exacerbated already existing burdens on the healthcare system, from overflowing emergency rooms to staffing issues. Stephen White, a commander at Austin-Travis County EMS in Austin, Texas, oversees a community paramedicine initiative known as the Collaborative Care Communication Center (aka C4). He says the program has significantly alleviated that pressure.
“One of the problems that you’re seeing across the country are hold times, where an ambulance will transport to a hospital, but then they can’t unload onto the hospital staff for an hour, two hours, three hours sometimes,” White said. “The EMS system that I’m in is very high-volume, very fast-paced. We will do 600 calls in a day. So if we incapacitate our crews for hours because they can’t offload patients, then we’re making it harder on everyone else in the system.”
 The patients who are getting held up are low-acuity patients, adds White.
The patients who are getting held up are low-acuity patients, adds White.
“EMS has changed so much. It used to be people only called EMS when they were dying. But now for a lot of people, 911 is the entry point into the healthcare system,” he said. “They don’t have the means to go see a primary care physician or to drive themselves to the hospital, even for very minor things. So they utilize 911.”
The C4 program is designed to handle those low-acuity patients, who, says White, are better served somewhere other than the emergency room. Through C4, Austin-Travis County EMS has been able to mitigate 51% of all patient contacts, and the agency conducted a total of 998 telemedicine consults last year, according to White.
The goal of community paramedicine models is to get people the care they need, whether in the ED or via alternative methods of care. From both a time and a cost perspective, telemedicine and treating in place aren’t just beneficial in urban environments but advantageous in rural areas as well.
Telemedicine and community paramedicine can help combat many of the challenges that come with working in a rural environment, where the nearest hospital or specialist can be a lengthy drive away. Bringing care to a patient’s location by enhancing what first responders are capable of doing on the scene, reducing time to care through telehealth consultations and expanding access to local health services by using telehealth can all help rural EMS agencies with limited resources better serve those in need by improving access to specialists and reducing demands on staffing and labor.
In particular, telemedicine facilitated by EMS can help bridge the healthcare gap by connecting patients to physicians for non-emergencies such as preventative care or treatment of chronic issues like diabetes.
COVID-19 has underscored the biological hazards EMS providers face on the job every day. The rise of telehealth during the past several pandemic years can be attributed in part to infection control and the ease of evaluating patients via technology, which can protect EMTs and paramedics from unnecessary exposure and cut down on time spent donning and doffing PPE.
One of the biggest questions about community paramedicine programs is how to fund them. ET3 is a game-changer in making it easier to get funding for some community paramedicine efforts. ET3, the Emergency Triage, Treat and Transport Model, offers Medicare reimbursement for certain services other than transports to emergency rooms.
EMS agencies can use partners like urgent care providers or doctors’ offices for alternative transports, treat in place and more fully take advantage of telehealth technology to bring a doctor’s “telepresence” to the scene. Although still very much in its infancy, ET3 has already shown promise to those who are piloting it, such as urban areas like Austin-Travis County – where ET3 is a component of the C4 program – and rural areas like Delta County, Colorado.
Partnerships are the bedrock of a successful community paramedicine program, and by nature, agencies implementing them form stronger relationships with health services like nonprofits, substance abuse treatment centers and urgent care providers. White says that adding value to partnerships has ensured successful referrals and collaborations within the C4 program.
“Our goal is to add value to that referral,” White said. “So we have a field crew that encounters a patient that calls C4. We identify that this would really be best with a long-term care facility.”

ATCEMS uses Pulsara to communicate with healthcare partners so that they can share a patient’s pertinent information securely before their visit.
“We do as much of the work as we can so that the referral is as successful as it can be,” White said. “By adding value to your referrals, into your partnerships, it adds value into your program and your partnerships are much easier. The success of that referral and what the partnership is able to do with it is really based on how much information you give them. If I just give that partnership a name and a birth date, that just doesn’t give them enough information.”
What does good telemedicine look like? According to White, video – not just audio – is crucial to effective evaluation of a patient.
“Having two-way video when doing telehealth is imperative – enabling the physician to see the patient, and on the patient side, being able to connect with the physician,” White said. “For example, you may have a patient who says their stomach hurts. Well, abdominal pain has a thousand different causes. If the provider says it’s the patient’s lower abdomen that hurts, it’s just not specific enough. The physician has to be able to see where the patient points their finger. Otherwise, you can play that game of telephone where information is moving around from person to person and you lose what’s important. Having video cuts through all of that.”
Telehealth can potentially add another avenue of options for providing service to high-acuity patients who refuse transport to a hospital.
“Let’s say you have a patient with chest pain,” White said. “It is very obvious they’re having a heart attack, but they do not want to go to the hospital. Before, you would say ‘Sign this document, you’re refusing to go to the hospital, we think you should go. Good luck to you.’ Well, now we have telehealth. Now you can bring a doctor into the call. The doctor can consult with them. Because we have the whole system set up to mitigate low-acuity patients, we can also mitigate these high-risk refusals.”
The consulting physician can request a specific follow-up time or send resources to the patient, expanding the options available during the EMS visit.
“Before, we weren’t able to offer them any other services during high-risk refusal,” White said. “It’s a very fine line, but it’s also very exciting because you’re able to do more for the patient that you haven’t been able to do before.”
COVID-19 has created numerous challenges, but as the world has been forced to adapt, some positive developments have come out of the crisis, particularly in terms of accelerating innovation and adopting new ways of working and interacting.
One of the concerns surrounding telemedicine in the “before times” was buy-in, both from the community and from health providers. But in the past few years, it’s likely that you and most people you know have at some point used telehealth, whether professionally or personally. Telehealth isn’t novel anymore, and implementing it as part of a community paramedicine program from a buy-in perspective is no longer the hurdle that it was just a few years ago.

Data is key both in the initial stages of setting up a community paramedicine program and during the program itself. What categories of calls are adding significant stress to the EMS system in your area? A needs assessment will illuminate those areas and inform which specific health partners you’re going to need to target for collaborations.
In the case of C4, some of the predominant areas that needed to be addressed through community paramedicine were calls involving people experiencing homeless, mental health crises and COVID-19 patients. Ongoing data collection, such as monitoring metrics like how many calls are being mitigated and tracking success, is just as crucial. This data will help your agency evaluate areas that need adjustments and generate ongoing funding for the program.
BONUS: Community paramedicine’s efficiency can help combat the gas crisis
As community paramedicine reduces the number of unnecessary transports, it can also help cut costs at the pump. Using less fuel has a direct impact on the cost of healthcare. No matter how long the current gas crisis goes on, this disruption won’t be the last, and using less fuel is advantageous even when prices are stable.
Cole Zercoe previously served as Senior Associate Editor of Lexipol's Police1.com and Corrections1.com. His award-winning features focus on the complexity of policing in the modern world.
![]()
Chronic stress may not seem like a big deal, but it has a variety of wide-ranging effects. Check out 10 Things You Need To Know About PTSD And Chronic Stress In EMS to learn more.

December Recap After an incredibly busy events year with 102 conferences, trade shows, and sponsorships, December was on the slower side for us, with...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)
Published research shows how using Pulsara, alongside standardized field activation and a focus on stakeholder relationships, improves STEMI care and...