Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

Editor’s Note: This post was updated in January 2025 for accuracy and comprehensiveness.
While the effects of the COVID-19 pandemic grow less dire each year, its impacts are still being felt by healthcare workers in all disciplines. For emergency service organizations, these lasting challenges take the shape of staffing issues, with fewer providers on the job than many service areas need. Year after year, staffing ranks among the most stressful parts of the job for EMS professionals, with 57% of EMS Trend Report respondents reporting inadequate personnel numbers to meet the demands of 911 calls. This critical, widespread issue is having real impacts on patient care and the well-being of providers.
Over the past few years, telehealth has become a favored tool in non-emergent care for helping clinicians treat patients from a distance. However, many EMS organizations are now discovering that leveraging telehealth as a part of normal practice can actually help save time, preserve resources, and increase the output of smaller crews.
If you're struggling with staffing shortages, here are a few ways telehealth may be able to help you work with the resources you have.
While the drawback to telehealth is that virtual encounters are not always as thorough as in-person ones, telehealth does offer a key advantage: allowing one person to be present in multiple places over a brief span of time. Combined with the fact that some low-acuity calls can be solved without a provider on-scene, telehealth can be a formidable tool to help fewer medics assist more people in a shorter amount of time.
Telehealth allows calls to be conducted more quickly—either by eliminating the need for transport, or by giving the medics more information before they arrive. Using telehealth to attend to low-acuity calls maximizes the time spent with the patient by saving time that medics would normally spend traveling to and transporting the patient. This frees up medics and high-demand resources to go where they're needed when they're needed.

Clinicians in Teller County, Colorado, are using telehealth as a force multiplier to expand the sphere of power for their EMS teams. Ute Pass Regional Health Service District covers a large area with limited resources. When faced with COVID, explained James McLaughlin, UPRHSD's Director of Community Paramedicine, they needed to get creative: “With our current workforce, we run three ambulances and cover 539 square miles. There was no way we were going to be able to meet the potential demand of COVID without coming up with a unique and interesting way to address it.”
They found that setting up each individual provider inside the ambulance with the ability to conduct calls via telehealth was an immediate force multiplier for their resources. McLaughlin explained: “We were able to take these ambulances, split up a crew, and have one crew member run one call while another crew member runs another call. It becomes a force multiplier for us. We can take one ambulance and double the output of that crew.” When not every call needs 911 response on the scene or transport, empowering medics to start a telehealth consultation to determine the appropriate next steps can help save both time and resources.
Not all patients need transport to the hospital. A telehealth consultation can help distinguish calls that will need transport from calls that can be solved via telehealth, as well as provide a better, more detailed flow of information sooner in the process. Austin-Travis County EMS in Austin, Texas, has recently begun leveraging their elite C4 team of medics to help coordinate care for low-acuity calls, allowing them to quickly determine the most appropriate solution for a patient's problem and dispatch resources accordingly. Not only does this save time and resources, but it also helps provide the patient with the best possible care in a timely manner.
Several emergency services organizations across the United States have found a way to take telehealth's weakness—strictly virtual patient encounters—and turn it into a time-saving strength.
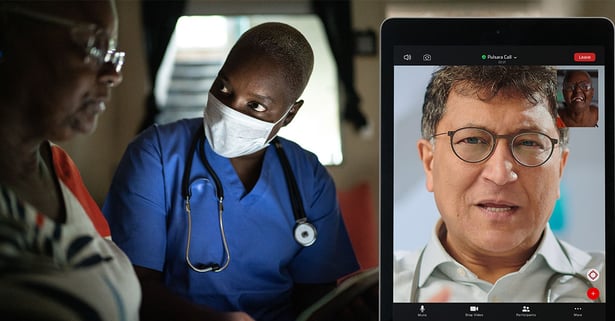
Organizations are equipping their medics with telehealth tools and empowering them to reach out to their medical directors or other physicians on-call for telehealth. Once on-scene, the medic can do an initial assessment of the patient and then initiate a telehealth call with a physician. They can allow the physician to see the patient and describe their own analysis, and from there, the medic and physician can work together to determine the best course of action for the patient.
This helps facilitate treatment-in-place, which can help cut down on transports, saving medics time and hospital beds. It also enables a more comprehensive and accurate flow of information between providers, ensuring that patients receive the highest level of quality care.
Staffing shortages make it difficult to effectively meet the needs of the community. However, one thing that can help manage call volume is improving the overall health of the community. And yes, community paramedics can help work toward this goal by leveraging telehealth.
911 isn't the most appropriate solution for every problem. However, it is the clearest and most accessible path for most patients to seek help. This often results in patients who frequently call 911 to get help with a specific problem, and often receive transport to the hospital—even if that isn't the most appropriate destination for their problem.
Community paramedicine programs are designed to meet patients where they are, identify problems that an emergency room can't solve, and provide patients with personalized care that gets to the heart of their experience. Community paramedicine programs across the U.S. are starting to leverage telehealth as a way to do just that.
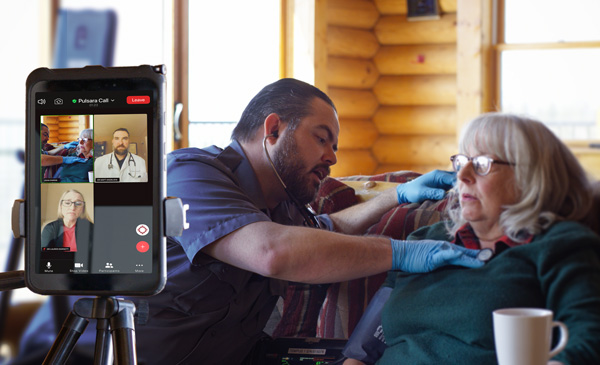
By giving paramedics the ability to connect with a wide range of providers—medical directors, physicians, nursing homes, clinics, community health resources, or mental health—while still on-scene with a patient, telehealth can help facilitate better care for patients. This approach to care improves the overall health of the community and helps solve future incidents before they happen.
Teller County's community paramedics have seen a great deal of success with this strategy, as patients who otherwise would not have received care by a board-certified emergency medicine physician have received care in their home, and have been given access to medications, referrals to primary and specialty physicians, and other community resources.
To learn more about how Teller County's community paramedics have been using telehealth to improve care for their patients, check out their case study on the subject.
Telehealth is one of many ways that communication technology can ease the burden of staffing difficulties. Pulsara is a healthcare communication and logistics software that unites EMS and hospital teams on one scalable platform. From everyday emergencies to mass casualty incidents, learn more about how Pulsara can streamline EMS communication here.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...