Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
11 min read
 Team Pulsara
:
Jun 02, 2021
Team Pulsara
:
Jun 02, 2021

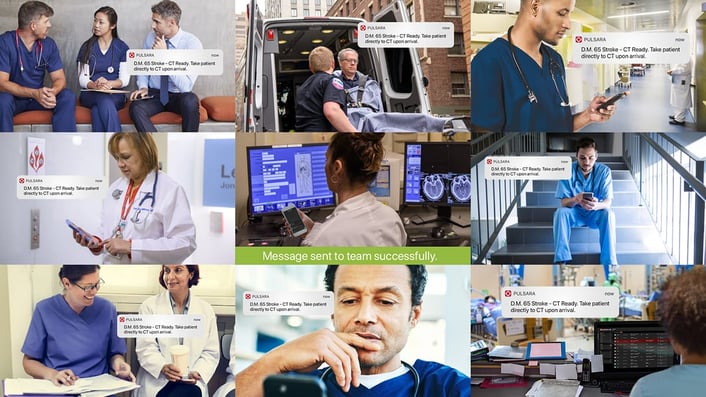
Patient care involves many moving parts, several teams, and a lot of people. How do you get everybody on the same page, especially when messages have to travel through multiple communication methods before they reach their intended recipient? How do you unite all the disparate teams involved in a patient's healthcare journey—from ambulance to emergency department to specialty teams—into one region-wide system of care?
Over the last few years, a group of leading experts and clinicians in Victoria, Australia have implemented cutting-edge technology to improve communication between their care teams. They've seen a great deal of success with their strategies, and have developed a streamlined system for making sure everyone on the team has the right information at the right time.
In this three-part series, you'll hear directly from them on their search for a solution, the results they've seen, and the advice they would offer other systems that want to build their own regional system of care.
View the full webinar video discussion below, or read on for Part 1 of the full roundtable! (Part 2 and Part 3 can be accessed here.)

Kris Kaull: Hi there, greetings and welcome to this exciting webinar. My name is Kris Kaull. I am a critical care flight paramedic out of the U.S., as well as a technologist in marketing. I am so blessed to be at this round table of amazing folks with us. Today's topic is about creating a regional system of care and how these leaders, along with their comprehensive medical teams changed how they assess and treat patients. Today we're going to be talking about their systems, the challenges they faced, what they changed and implemented, and the outcomes they've seen.
As you can see, we have a great group of panelists. We have leaders in nursing, academia, neurology, and the ambulance prehospital arena. Our objective today is to talk about healthcare, but not the four walls of the ambulance, or the four walls of the surgery suite, or the four walls of the emergency department. Instead, we're asking, how do you build an entire regional system of care?
If you think about it from the perspective of the patient, they aren't isolated to any one of those care spaces. They start maybe at the home, and they're transported, and during their journey through there, their care happens with a lot of moving parts and a lot of people. How do you get all the members of the care team on the same page?
Dr. Bladin, a few years ago, you started looking at how to best tackle some challenges you face. Can you share a little bit about the clinical landscape and some of the challenges you were looking to solve?
Chris Bladin: Yeah, that's a great question. We started thinking about this way back in around 2013 or 2014. The thing that struck me was that when new stroke patients had to come in quickly, the communication between the outside world, the community world, and the hospital was key. There was hospital pre-notification about patients coming in, but it was clear to us that that was difficult. It was patchy—and certainly in the regional environment, which I was increasingly starting to work in—it was, can I say, less mature; maybe less sophisticated than it was in a metro environment where a lot of those systems are embedded. So I was really looking at that time to utilize digital technology and digital health apps to try and facilitate that. I did a scan of the landscape and back in those days, there wasn't a lot around.
By going to conferences and just talking to people I ran into James Woodson, who is the CEO of Pulsara. Pulsara was a much smaller entity back in those days, but by about 2014 or 2015, it was clear that this was something we really needed to test out.
Our approach into this was in keeping with my background, which was: we need to do some research into this. Does this work? It looks good. I'm a nerd; I love this stuff and I would love to use it, but that's not the same as, "Is this actually going to be beneficial for patients? Is it going to be beneficial for and reduce complexity in the communication processes between ambulance and hospital?"
So that led us to a grant into the Heart Foundation, and we followed it up with a research grant into the Stroke Foundation. To cut a long story short, we established Pulsara and tested it out across two key hospitals: Bendigo and then Ballarat Hospital in regional Victoria. That research project went for several years.
Katie [Dr. Bagot] was the rock star in that process in terms of organizing the implementation of Pulsara—keeping everyone on track, keeping the research protocols tight. And I should add the Pulsara team— without wanting to talk them up too much—but they were fantastic and they came out to Australia and did a number of site visits and really helped facilitate the implementation into both ambulance and hospital.
And the key thing about this is that it's all very well to ring ahead into the hospital and the ED to let the emergency department know that you're coming in, but the communication reach has to be so much further. It has to really go into those core components of the hospital that are going to actually impact patient care.
So for us in stroke, that is notifying the people in the CT scanner that there's a patient coming in, notifying the docs on the floor in the regional hospital that there's a stroke patient coming in and we could be giving thrombolysis, so they need to get down to the ED and quickly assess the patient. It's that ethos of "time is brain" that we really wanted to address.
"We found the door-to-CT time was about 44 minutes faster, and door-to-PCI,door-to-balloon times for STEMI was improved by at least 17 minutes."
Now, my background is stroke, but stroke is a small part of emergency admissions to the hospital. At that time, Pulsara was geared towards stroke and STEMI. So we took the sensible approach of, these two conditions have a lot that aligns them. Similarly, for STEMI, you need to reach into the ED, but you also need to reach into the cath lab for emergency PCI procedures for cardiac thrombosis, et cetera.
So the two conditions linked up very well, and we used that as the basis for starting this research project across the two hospitals to see whether that communication process would be improved. And we knew from research, particularly research that Katie did, that there can be 5 to 10 different phone calls just to convey information. And as so often with telephone calls, that information can get a little bit twisted, and the nuance of some clinical elements can change. And having everyone on the same page with the same information, which is what Pulsara does, is really a key for us.
I can go over the research, but we found really across the board that Pulsara improved the timelines in terms of processes of care. I mean, just to give one example for us in stroke, we found the door-to-CT time was about 44 minutes faster, and door-to-PCI, door-to-balloon times for STEMI was improved by at least 17 minutes. But there are a number of other processes of care that the timelines just got better and better. And that talks about pure metrics, but in many ways, it's the qualitative improvements that really made the difference. And what I might do Kris, is perhaps throw to Katie just to talk about the qualitative elements of this, because it's Katie's area of expertise.
Kris Kaull: Yeah, that's a great lead-in, because that was my next question.
I think that you said two things that were really important: number one, technology for technology's sake may be fun internally, but it really has to impact patient care. And number two, the way that we do things clinically is not how we communicate in real life, right? I don't emergently fax a grocery list to my son to pick up milk, and I don't page Katie to see if she wants to connect with me later after work. Yet that's how we communicate during a time-sensitive emergency. Everyone's looking for that magic bullet, the quick fix: buy this product, enable this leadership strategy, stop doing this, start doing that. But Katie, as the Ph.D. doctor in the group and the one who tracks change and tracks the data, can you speak a little bit to implementing those changes and that strategy?

Kathleen Bagot: Yeah, definitely. So as Chris said, it really was a multidisciplinary approach that we took to looking at Pulsara and implementing it. And one of the first things that we did in terms of implementing change was to look at it from two different perspectives. One was from a system level, and one was from an individual level. On the system level, we got everybody from all of the different areas in the same room: prehospital, ED, triage, radiography, cardiology, urology, and everybody across to talk through the process from start to finish as to how communication currently worked. Then everybody got an understanding of where everybody was at and how it all worked.
And even during that process, we found that change already started happening, because people in the room were going, 'Oh, I didn't know that that's why you did that.' Or, 'Oh, is that why that takes so long? We didn't know that, we just thought you were just dragging your feet!' So there was all of this interdisciplinary understanding that came from that.
"We tracked every single time point for the patient care journey from prehospital through to the delivery of care. ... That then allowed us to evaluate what was happening at each stage, and then, after the implementation of the app, to be able to see where it had improved, where it hadn't, and be able to investigate case by case, but also at an aggregate level."
And then we looked at it from an individual perspective. I spoke to different individuals across all of those different areas. We did a whole lot of surveys with those individuals as well, to ask about what worked and what didn't, so that we understood the current communication processes and the current things that did and didn't work. And then we also asked them about Pulsara, or about a single communication system. What did they think the benefits of that would be, and then what would the concerns be? We wanted to understand the possible factors that would help change, or inhibit or delay change. And then we tracked every single time point for the patient care journey from prehospital through to the delivery of care. We have to go to multiple systems to find that data, so it was time-intensive and tricky. But that then allowed us to evaluate what was happening at each stage, and then, after the implementation of the app, to be able to see where it had improved, where it hadn't, and be able to investigate case by case, but also at an aggregate level.
Kris Kaull: We'll get into some of the data as well here in a moment. Janet, you were really on the implementation side for Latrobe Regional Hospital. Streamlining communication was a big focus, both to improve patient care, but also to strengthen that collaboration with all those involved. Up until the beginning of 2020, Latrobe Regional used a combination of phone calls and pagers to interface between emergency services, the emergency department, and hospital staff. Can you speak to that implementation strategy and that outcome?

Janet May: Sure. So in early 2020, we brought in Pulsara for pre-notification. We used it mostly for acute time-critical patients. You can use it for everything coming in, but we were aware that we didn't want to over-alert the emergency department. So as Chris said earlier, we had it set up for the stroke teams, trauma teams, and STEMI's that were coming in. All would receive the same information that the Ambulance Victoria crew had put on Pulsara. And we've also expanded it as well now, so we use it for our inpatient strokes on the wards.
I think overall the best outcome we've had is quicker treatment times for patients because it's really streamlined our communication, right from pre-notification into the ED and then to our internal teams. One of the big things we noticed was the improvement in the accuracy of the patient demographic data coming in. We used to have a bat phone, or we still do have a bat phone for backup. It was a dedicated phone line that the ambulance would use to call in for anything acute time-critical.
"The best outcome we've had is quicker treatment times for patients because it's really streamlined our communication, right from pre-notification into the ED and then to our internal teams."
So the way that would work is the Ambulance Victoria crew would have to call center control, who would then call us on the bat phone with what was coming in. And if we had to clarify any details, or sometimes in outlying Gippsland areas there are phone services patching, and you'd miss their name. We couldn't clarify any of that until the patient was on the doorstep. So now we have all that information and we've reduced all those data errors. And also for those patients, you get a lot more clinical information on Pulsara than just a name and a date of birth and that it's a stroke or trauma coming in. We think it's actually less than the administration work that we've had to do with multiple phone calls once the patient comes in and then nursing charge would have to initiate a stroke page and then call the surgeons in theater, if it was a trauma. So all of that's gone, and they just flipped the Pulsara notification to the team, so they're all on the same page at the same time.
Kris Kaull:
Yeah. And having everyone on the same page at the same time is so important. Grant, we've talked in the past about how you have a great, established relationship between the ambulance crew and the paramedics with the emergency department. They're great, but you really are the backbone of out-of-hospital medicine, both in the urban cities and the rural countryside. And there's a major role that paramedics play in this regional system of care. Tell me a little bit about how those relationships have changed over the last few years as you guys have implemented this regional team approach.
Grant Hocking:
Thanks, Kris. Yeah. So we've always had, as you said, a great relationship with the hospitals through the emergency departments, and that hasn't changed. The paramedics know the emergency staff quite well, get on very well, and have a good relationship, and it doesn't really extend beyond the ED, in most cases. And that relationship hasn't changed.
In the past, when we would let the ED know we were bringing in a time-critical patient, we did that, as Janet has said, via radio or phone—via a third party in our communication center, usually the clinician. And we would include things like vital signs, medications, allergies, patient name, sometimes date of birth, and UR numbers, things like that.
"We're all working together much better. So the relationships are vastly improved.Everyone feels more empowered. We feel more confident."
But typically, as professor Bladin mentioned, once it went beyond the ED and they went to let somebody else know, they'd always just basically get told: "there's an 83-year-old female with stroke coming in." They wouldn't get all that other information. And that was a regular occurrence for me at the Stroke Clinical Network meetings, getting asked, "How come they only told us the patient's age and the presenting condition?"
So yeah, there were communication issues there. But now obviously our patient notification has improved significantly. We feel like we're more part of a greater team that includes neurology, radiology, cardiology, and medical specialists. So it's a bigger scope now, and the messaging obviously exceeds beyond the emergency department. So we're all connected at the same time, which is brilliant.

For us as paramedics, that means a lot, because we're about patient-centered care and delivering the best care for the patient. It gives us a lot of confidence to know that now in the background everything's being done as much as possible to get ready for the patient's arrival.
And we've seen the results. The care is much more immediate and the patients do have better outcomes. Everyone can see the patient's details. We can now transmit ECGs in much better quality than what we are doing in most other parts of the state, which is using fax machines. We have immediate communication that enables us to receive and ask questions, and we can send in more details as we get them. We're all working together much better. So the relationships are vastly improved. Everyone feels more empowered. We feel more confident. We know the staff at the hospitals can see the results themselves. So we're all more confident and more empowered, everything's transparent, more immediate. It's just a much better system than what we were using.
Chris mentioned a couple of the results, but for us at Ambulance Victoria, we were getting patients off stretchers five minutes quicker than without Pulsara. We were clearing hospitals 10 minutes quicker than without Pulsara. So on our side of things, that made a huge difference. For the patients, Chris mentioned the door-to-CT scan for stroke patients is 45 to 51 minutes quicker. Door-to-needle times are much quicker. And we've got a target time of 60 minutes for stroke patients to get thrombolyzed in, and our numbers there more than doubled. We went from 11% up to 25% of patients getting thrombolyzed within that 60-minute target window. So the outcomes speak for themselves, really.
Kris Kaull:
Yeah, this is so great. It sounds like I paid each and every one of you millions of dollars to say all these great things about Pulsara, but that's not true. In fact, not everything is perfect and not everything goes as planned. And yet at the end of the day, it really is about doing the right thing for the patient and being on the same team.
What advice will the panelists give to those looking to build a similar regional system of care?
![]()
St. Dominic Hospital in Jackson, Mississippi, recently announced that they have pioneered an innovative new cross-departmental triage protocol that leverages the Pulsara platform to improve care team communication and patient care. Check out the details here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...