EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, John Erich, for EMS1 BrandFocus Staff.
Once you’ve determined what your program will do, you face some practical questions
The proverbial table is set, and you’re ready to begin your EMS agency’s community paramedicine program. You’ve evaluated the needs of your patients and community, identified care gaps you can fill, planned how you’ll do it, and lined up appropriate partners to assist.
Now, however, you face a new round of challenges – and these are more practical than theoretical. Who will comprise your team? What tools will they carry? How will they communicate and document care? And, once they’re out in the field and helping people, how will you evaluate their success?
Alexandria Fire Department in Alexandria, Virginia, chose fall prevention for its initial foray into community paramedicine back in 2017. Focusing on falls made a lot of sense for a new program with limited means: Data on local frequent fallers was available and accessible, and the interventions that could help them – good shoes, handrails, securing rugs, controlling pets – were low-cost and straightforward. The program would be a manageable lift to get off the ground.
And, given its targeted scope, easier to keep upright as it found its footing and began moving forward.
“You have to figure out what’s easy,” said Jeff Woolsey, a department captain and registered nurse who took over Alexandria’s program in its early days. “Pick something you know you can succeed at – and falls are something you can succeed at. If you go out there and say, ‘I want to solve mental health! I want to solve drug addiction!’ you’re going to lose. There’s just no way, without 14 people in your program and a 10-bed hospital someplace, that you can manage those things.”
WHAT MAKES A GOOD COMMUNITY PARAMEDIC?
Woolsey didn’t have a CP background when he inherited Alexandria’s nascent program. But he was generally the type of provider you want for such an endeavor. Beyond the RN qualification (not essential but a valuable bonus), he had soft skills – he enjoyed talking to people. And as a veteran paramedic, he knew how to break the ice and spark a conversation.
“I loved getting people in the back of the ambulance and, if it wasn’t something serious, talking to them,” he said. “With elderly people I’d ask, ‘Hey, you’ve been married 50 years – what’s the secret?’ With men I’d always ask about their first car – every guy always wants to talk about his first car. It was a great way to open the door and get them talking.”
Alexandria Fire staffed its program with volunteers – no one was drafted, and that ensured its CPs wanted to be doing community paramedicine and had their hearts in it. In any department, not everyone is cut out for reminiscing about a senior’s beloved ’52 Pontiac.
If you’re a chief or team leader charged with staffing a new CP project, certainly look at clinical skills, but also to your medics who are chatty, curious, and perhaps take a bit more time on scenes. While those attributes aren’t always positives in the 911 world, they fit well with community paramedicine, where you want providers who can gain trust and ferret out underlying problems.
“I’ve had people tell me I’m easy to talk to,” Woolsey acknowledged. “But it takes a lot of mental energy, I think, to talk to elderly people, to try to help them figure out what can benefit them. It can be a little tiring at times, especially when you do it every day.” Recruit those with a temperament for it.

WHAT TOOLS WILL CPS NEED?
What community paramedics carry on calls may vary a bit with their program’s mission, but the basic paramedic medical kit is usually still appropriate – remember, CP patients may be elderly, vulnerable, and have comorbid conditions and unfavorable social determinants of health. You may not need a full drug box or complement of ambulance gear (many CPs operate in fly cars with limited space), but some core lifesaving tools are probably prudent too. Other items will be tailored to program needs.
“I carried a first aid kit and a Lifepak 15,” recalled Woolsey. “I went out and bought some Gorilla tape because it was good to have to tape down things like wires, cords, and the edges of rugs.”
Alexandria had no actual budget when it started, though it absorbed small costs here and there – overtime for its CP volunteers to conduct visits at the ends of their shifts, a new backpack for Woolsey after two years. But of course money is perennially tight in EMS, so providers paying for smaller incidentals like tape out of pocket isn’t unusual.
A valuable “tool” that might be overlooked is transportation. Community paramedicine arose in part as a response to superutilizers, many of whom simply called 911 repeatedly for basic medical transportation needs – to get to a hospital appointment, for instance, or even a pharmacy. Arranging alternative ride options for such patients is a core piece of many programs.
EMS agencies may be able to provide bus passes or reach agreements with taxi or ride-share companies to move these patients more appropriately.
HOW SHOULD CPS COMMUNICATE ABOUT CARE?
With the rise of community paramedicine has come new software options to help CPs chronicle care that’s ongoing, not one-and-done, and can involve a range of partners. Traditional patient care reports may suffice to get started, but those running bigger programs may find it worthwhile to invest in something more.
Woolsey notes that community paramedic-type calls “revolve around the client more than the incident” – an important distinction to keep in mind when selecting a software product.
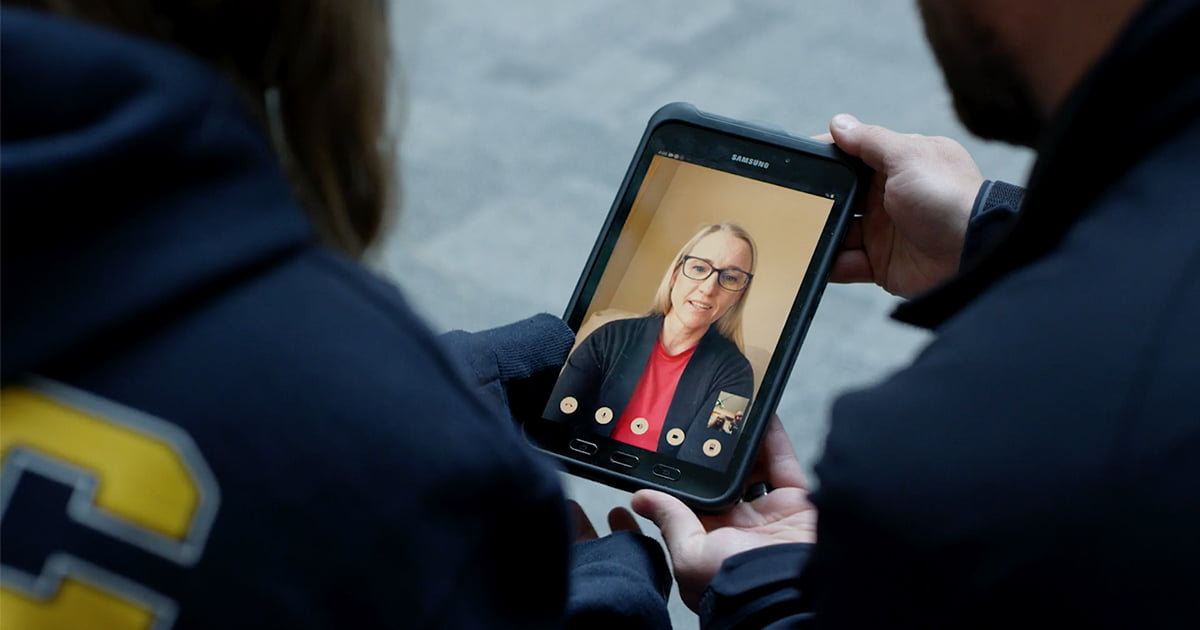
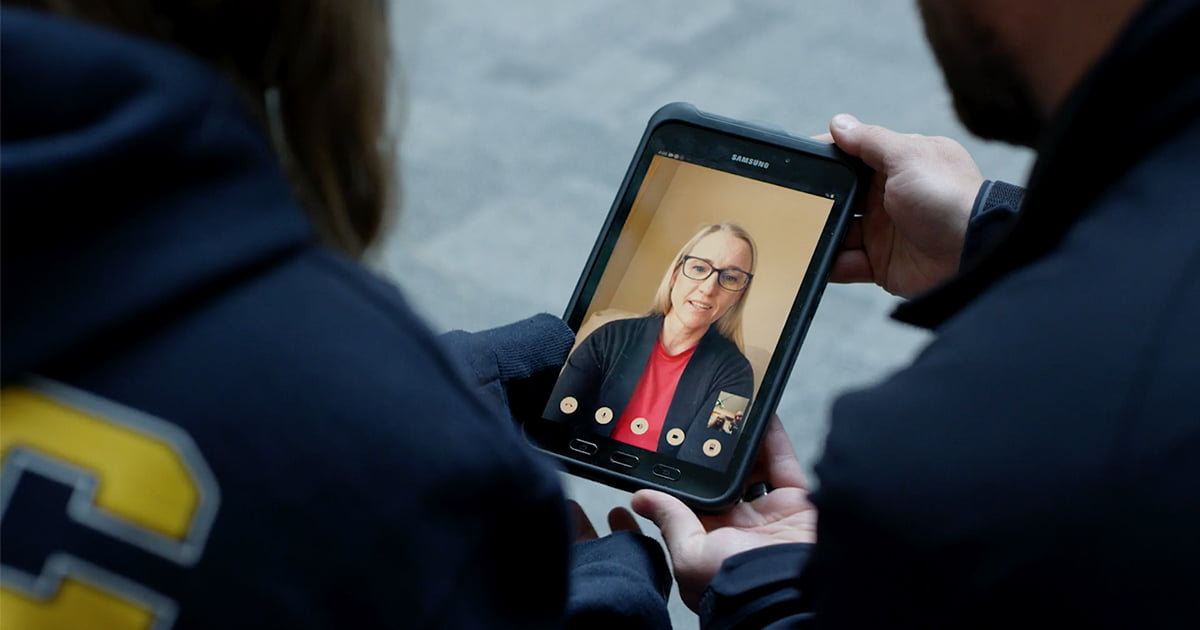
Pulsara can link all the providers on a patient’s care team in real time via a single secure, HIPAA-compliant platform that any new provider can join, see and update as a patient’s care progresses. It provides CPs and others on care teams a current, comprehensive view of all that’s been done when and by whom, thus making their own care faster and more appropriate. With Pulsara, CPs have the option to connect with physicians, specialists, and community partners instantly via live video, giving them the option to seek a physician’s input to medically clear behavioral health patients on the scene. Keeping community medics, other healthcare providers, specialists, and community resources all on the same page throughout the process reduces the risk of error, keeps patients happier, and makes everyone’s lives simpler.
HOW CAN YOU TELL IF YOU’RE MAKING A DIFFERENCE?
Whether a CP program is working is a story only partially told by data. Metrics like falls are easily measured – did a patient have fewer in the six months after intervention than the six months before? Did the community have fewer after the program was created than it did before? But that relies on cooperative patients who implement medics’ best-practice recommendations.
“It can be very difficult to decide if you’re making a difference,” said Woolsey. “I could point things out – you need to wear good-fitting rubber-soled shoes, you need to use transfer benches, you need to have your eyes checked – but I can’t force anyone to do anything. I can just suggest how to be safer.”
Successful programs, though, also improve lives in ways harder to measure. Woolsey and Alexandria Fire have done medication reconciliations for patients who didn’t understand their regimens and intervened when angry patients who misunderstood interventions lashed out at volunteers. They’ve linked needy citizens to household and food help. They’ve met and allied with county case workers, in one case helping obtain a guardian for a senior with memory issues who’d called 911 more than 200 times in a year. While their benefits may not be easily documentable, these ancillary activities improve lives.
The lesson, then, is simple but comes with a corollary: Start small, where your chances of success are high, and demonstrate benefit with data where you can – but if that’s not as clear and indisputable as you’d like, it doesn’t mean you’re not helping people.
“You might not have a tangible way of showing it, but just going out and educating the public on safety issues has great value,” Woolsey said. “People are amazed: ‘This fire guy came to my house and talked to me about this – I didn’t even know they had a program!’ And that engages them, and they’ll start opening up about other things. I’ve even had people ask for financial advice, which of course I can’t give them. But some of these people just need a little bit of life coaching, and that’s kind of what it comes down to.”

New advancements in communication and patient tracking technology are transforming response capabilities. Check out this exclusive webinar to hear emergency management and healthcare leaders from Texas and Colorado share how and why they're deploying these systems locally and statewide.
 Team Pulsara
Team Pulsara


![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)

