Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...
1 min read
 Brandon Means
:
Apr 20, 2016
Brandon Means
:
Apr 20, 2016
Defining Sepsis and Septic shock has been a hot topic since 1991, when the first definitions and clinical criteria for these conditions were published. After Emmanuel Rivers published “Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock” in 2001, the Surviving Sepsis campaign kicked off, significantly increasing awareness of Sepsis.
Since then, the consensus definitions of these conditions have changed multiple times. The question to ask is “Are we improving patient outcomes by changing the definitions?” If better defining syndromes like sepsis and septic shock is translating into adopting new treatments that benefit patients, it’s important that we stay up to date on these consensus definitions.
In 2001, the definition of sepsis (Sepsis-II) was simplified to the presence of an infection plus SIRS (systemic inflammatory response syndrome). Septic shock was defined as severe sepsis that was refractory to fluid therapy.
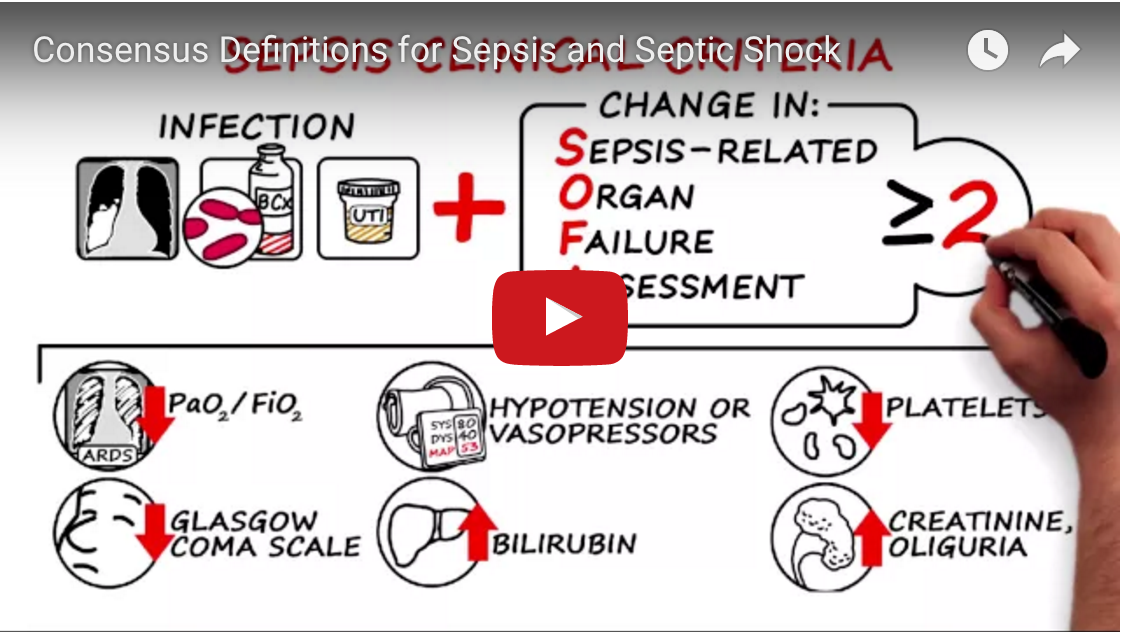
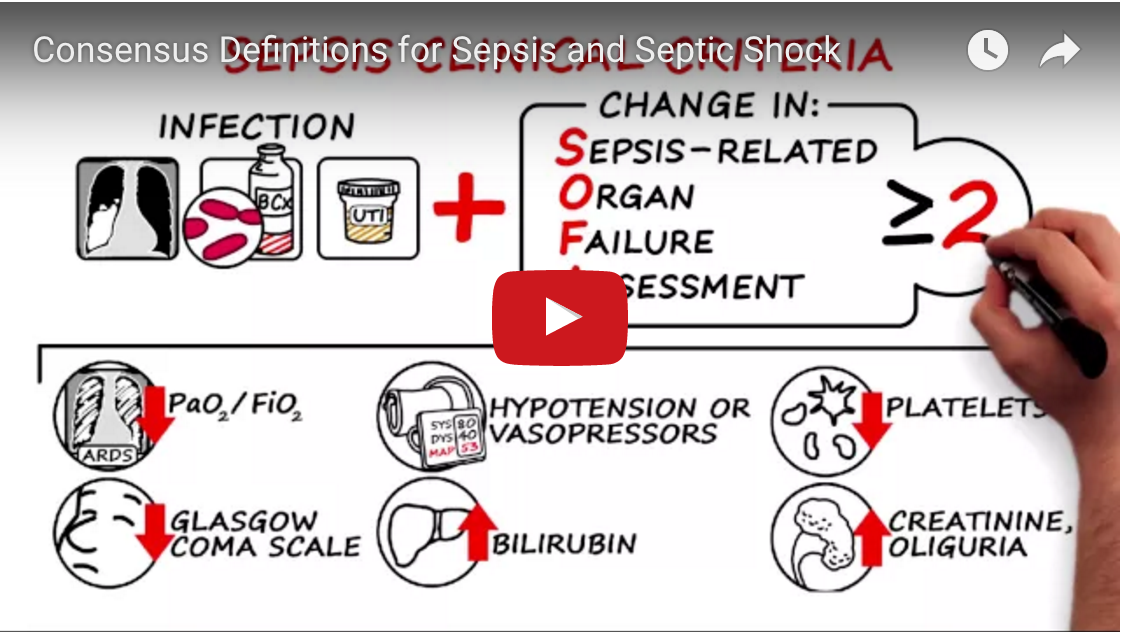
Now, in 2016, the third consensus definitions of sepsis and septic shock (Sepsis-III) have been published (see the differences between Sepsis-II and Sepsis-III here). When compared to the Sepsis-II definitions, the Sepsis III definitions replace the presence of SIRS with the SOFA (sepsis-related organ failure assessment) score. For areas outside of the critical care environment, a quick bedside score (qSOFA) is recommended.
When comparing the new consensus guidelines (Sepsis-III) to the old guidelines (Sepsis-II), there are a few things to consider. It may be a stretch to label the new definitions a “consensus,” at least in the United States. While the Sepsis-III definitions have been endorsed by the Society of Critical Care Medicine, the American Thoracic Society, and the Association of Critical Care Nurses, they have not been endorsed by the Infectious Disease Society of America, let alone any of the Emergency Medicine or Hospital Medicine Societies. Since sepsis is most often identified and diagnosed by an ED Physician or Hospitalist, this is hardly a consensus (according to PulmCrit).
What we do have a consensus on is the fact that defining and diagnosing syndromes like sepsis is, and should continue to be, a dynamic process that continuously evolves with new research. Since there is no magic number, lab value, or diagnostic tool to diagnose sepsis, knowledge of evidence based criteria, and willingness to challenge the status quo with new ideas and technology is key in improving patient outcomes.
For a detailed look at the new definitions, check out this video:
And for a comparison of the Sepsis-III definitions versus previous guidelines, the folks at EmCrit/PulmCrit have put out another fantastic article here, and JAMA released a thorough article detailing the changes here.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...