Does Your Team Feel Unseen? Close the Leadership Disconnect with 2-Way Communication
Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
3 min read
 Team Pulsara
:
Jan 05, 2024
Team Pulsara
:
Jan 05, 2024

EDITOR'S NOTE: This article originally appeared on FireRescue1.com. Special thanks to our guest author, Courtney Levin, for FireRescue1 BrandFocus Staff.
Now that you’ve developed the initial groundwork, these next steps are key to finding success
The fire service is pivotal in caring for their community’s underserved population. Introducing a community paramedicine program allows public safety to dynamically meet those needs.
Yet, developing and successfully implementing a community paramedic program can be daunting. “Generally, anytime you’re implementing a new program, specifically a community paramedicine program, the challenge is you’re doing something you haven’t done before – and there’s nothing more comforting than tradition,” said Kris Kaull, chief growth officer at Pulsara. “If you lead the change, it means you’re a disruptor. There’s certainly something glamorous about that, but there’s also something very disrupting about being a disruptor.”
Developing a community paramedicine program involves several steps before visiting your first patient. After creating departmental buy-in from the top down, thoroughly evaluating the medical needs of those in your community, and selecting a few specific areas for your program to focus on, it’s time to put your plans into action. Yet even if it appears that your department has crossed every t and dotted every i, you might still find the execution of your program doesn’t start smoothly.
WHEN THINGS DON’T GO ACCORDING TO PLAN
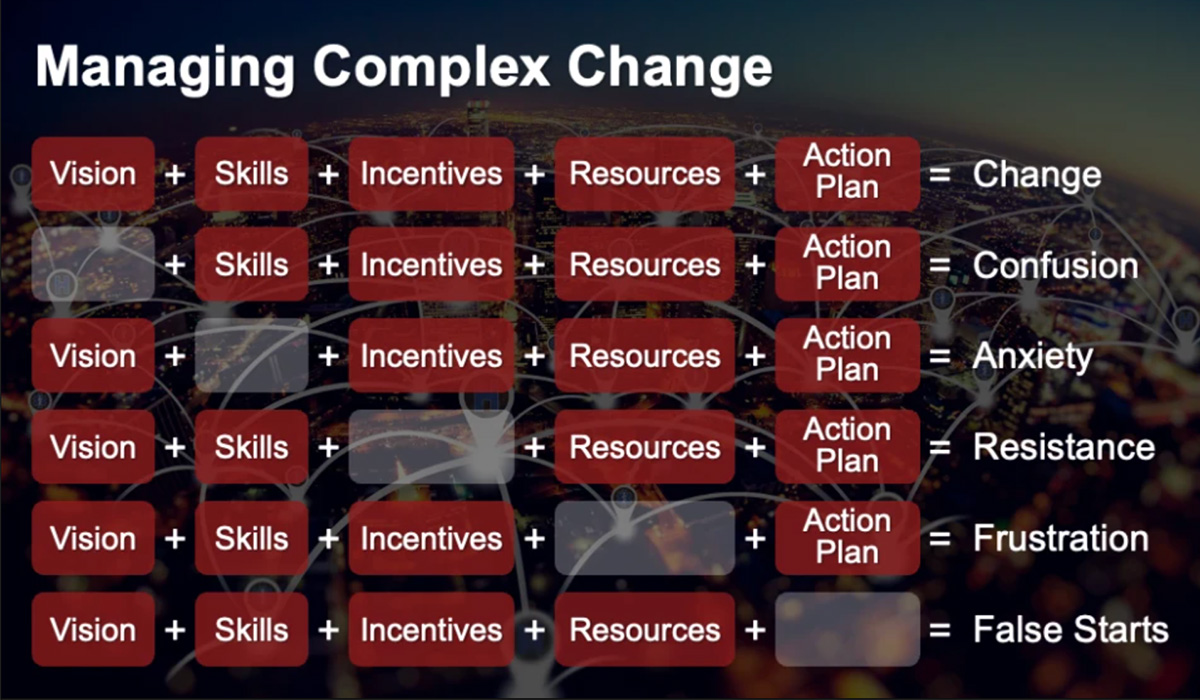
During the first few weeks or months of your community paramedicine program journey, you can expect frustration and confusion. Creating – and maintaining – a community paramedicine effort is complex. To help manage it, departments should focus on five key areas recommended by leadership expert Dr. Mary Lippitt:
RELYING ON ADDITIONAL EDUCATION
Vision, skills, incentives, resources, and a plan are all critical to a successful community paramedicine program. Still, one in particular – skills – may not always be able to be accomplished in-house. Discussions around vision or an action plan can happen at any place or time, but it’s the clinical education and experience required to meet the needs of underserved community members that may prove challenging for your department.
Fire departments should encourage and support their community paramedics to complete specific training and pass a community paramedic exam.
Offered through the International Board of Specialty Certification, the CP-C exam will help ready firefighters to take on the expanded scope of patient care that comes with being involved in a community paramedicine program.
Unlike traditional education, which focuses on a patient’s immediate medical need, community paramedics may frequently assist with longer, more complex, chronic illnesses. As your program grows, so will the need for your team to obtain training across a wider range of medical conditions.
EVALUATING YOUR DEPARTMENT’S PROGRESS
With the right training, tools, and plan, your department is ready to launch its community paramedicine program. But how do you know if your program is truly effective? Developing an evaluation plan can help your agency determine the value of your efforts and help identify areas for improvement.
“One of the best things to do is start with a baseline data set,” said Kaull. “As an example, consider patients who routinely use 911 and are consistently transported repeatedly. How many patients did you transport more than once over the last year? How many of those can we highlight and help explain why we were transporting them?
“If we understand the underlying problem, we can work with specialists to get those patients the needed help they deserve. Then, track patient outcomes. By reviewing the data, it’s possible to objectively identify whether the program is making a difference.”
But how do we communicate with the right specialist? How do we follow up with patients? Many in the fire service rely on the Pulsara platform during emergency medical situations to streamline the collection and dissemination of patient information. In addition, Pulsara is often used for real-time video communication during situations that community paramedics often encounter.
Pulsara allows firefighters to establish a line of communication with various providers depending on each patient’s needs. Whether first responders need a real-time dialogue with a patient’s primary care physician or a referral to social services, they can track patient data through the easy-to-use platform.
By reviewing patient interaction information through Pulsara, departments can better understand the effectiveness of their community paramedicine program. Evaluating the pilot phase of your program by analyzing your data in conjunction with exploring what lessons other departments have learned will be the ultimate key to your success.
“Continual reevaluation of your program is key,” said Kaull. “A least quarterly, ask yourself what things are going great, what things aren’t, and what you should keep doing.”
![]()
For more ideas on how to kickstart a community paramedicine program in your fire department, check out Community Paramedicine: Where Does The Fire Service Fit In?

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....
![[PRESS RELEASE] Published Research Finds Up to 31% Faster STEMI Treatment Times in Rural Hospital Setting with Pulsara](https://www.pulsara.com/hubfs/_1_website-page-blog-assets/pulsara-hosp-teams-assign-cardio-stemi-rn-1200x701.jpg)
Published research shows how using Pulsara, alongside standardized field activation and a focus on stakeholder relationships, improves STEMI care and...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....