Baker to Vegas: Leveraging Pulsara to Manage a Planned Event
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

Make a plan for treating pediatric pain that includes managing unfamiliarity and stress in both the patient and their parents or caregivers
EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, Jonathan Lee, for EMS1 BrandFocus.
__
The most complete definition of pain is “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” (IASP). It is a highly complex and subjective condition in any patient.
With pediatrics, this complexity is intensified by the fact that paramedics don’t encounter pediatric patients as frequently, creating more unfamiliarity and stress. Challenges related to paramedic training and exposure to pediatrics often lead to myths and misconceptions. Here are 10 important things every provider should know about managing pain in children.
Pain is common in children, with more than a third of out-of-hospital pediatric patients complaining of pain. Two-thirds of that pain is described as intense or severe (Galinski et al 2010). Despite this, children often go without analgesia in the prehospital environment (Rutkowska & Skotnicka-Klonowicz 2015).

This trend is not limited to the prehospital environment. One study of emergency department patients with long bone fracture or burns showed that young age (6 months to 24 months) was associated with receiving no analgesia (Alexander & Manno 2003).
Poorly managed pain has consequences well beyond the patient’s time in the back of the ambulance. Alterations in brain development and stress response can persist throughout childhood, and even routine procedures in the very young can alter future pain perception (AAP 2015).
While there are many theories, the biopsychosocial model suggests that all illness has three major components (Engel). The model has direct applications to understanding and treating pain:
Age and level of development have important impacts on how pain is experienced by children. Biologically, there are big differences within the nervous system (especially in newborns). For example, newborns have a weaker inhibitory nervous system. In adults, this “turns down the volume” on noxious stimulus once it has been received by the brain.

Psychologically, a child’s ability to understand pain develops along with age and experience. Limited communication skills make describing pain more difficult. Socially, children rely heavily on parents and caregivers both for support as well as cues on how to navigate new situations.
The benefits of painful procedures such as blood glucose checks and IV starts require careful consideration. Will the procedure improve the care provided to the patient? Will deferring the procedure to the hospital put the patient at increased risk?
Children with a history of highly emotional responses to pain experience more distress during IV initiation and may benefit from having the procedure done in the more controlled environment within the hospital (McCarthy, et al 2010).
Being able to identify and quantify pain is important. The verbal numeric scale – “On a scale of 1-10, how bad is your pain?” – is a common tool for paramedics, but it may be developmentally inappropriate for younger children who can’t yet quantify their pain with a number.
In this case, a number of published tools, such as the Oucher and FACES scales, use pictures to help young children identify their level of pain. These tools are readily available and are easy to use (Principi 2018). A variety of scoring systems are also available to patients who are nonverbal due to either age or medical condition. If these tools are not readily available, a simplified VNS – “Are you having a little bit of pain or a lot of pain?” – is also an option. Parental perception of pain may also be helpful (von Baeyer, et al 2013).
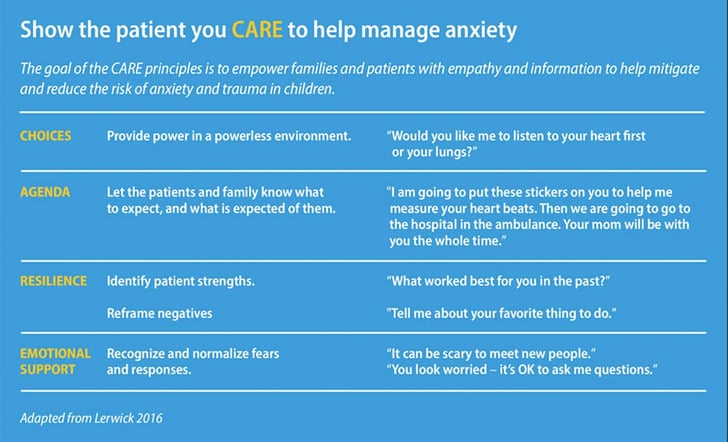
The influence of anxiety on pain is incredibly complex, and it extends beyond the patient. One example of a simple approach to minimize this anxiety is the set of CARE principles shown in the table below (Lerwick 2016).
The higher the level of anxiety, the more the patient will benefit from intervention. Parent needs should also be addressed, as higher parental anxiety leads to a higher level of distress in children as well (McCarthy, et al 2010).
Basic comfort measures, such as bandaging, splinting and ice or heat, are available to every level of provider and should not be overlooked. Deep breathing, nonprocedural talk, humor and coping statements are beneficial when used by providers and parents alike during needle-related procedures (Campbell 2017). Distraction is also effective during painful procedures (McCarthy, et al 2010).
In neonates, a number of simple interventions have been well researched. Consider swaddling, providing a soother or allowing the baby to breastfeed during procedures such as IV starts. These interventions have demonstrated to reduce crying time and heart rate (AAP).
Pain that is refractory to initial treatment steps should be evaluated for non-narcotic analgesia. Broadly speaking, these fall into two categories: acetaminophen and non-steroidal anti-inflammatories (NSAIDs). Both classes of drugs provide analgesia, but through different mechanisms. For example, acetaminophen does not have the anti-inflammatory properties of NSAIDs. This means that acetaminophen can typically be given simultaneously with an NSAID to improve effectiveness.
In newborns, 24% oral sucrose has been extensively studied and provided two to four minutes of analgesia for use with painful procedures (AAP). It is often packaged in 1-2ml containers so that it can be administered one drop at a time. While these are not commonly found in the prehospital world, dextrose solutions of 20-30% could easily be prepared from an amp of D50W and are proven to have a similar effectiveness.
Commonly available narcotics include drugs like hydromorphone, morphine and fentanyl (Principi 2018). These strong opioids are generally reserved for moderate to severe pain, as they tend to have more immediate side effects.
As their name implies, narcotics generally provide analgesia as a result of their actions on opioid receptors. This class of drug is not better or worse than other forms of analgesia, it is just different. Pain relief can often be improved by combining narcotics with acetaminophen or NSAIDs.

Having a stepwise approach to managing pain means treatment will be consistent and comprehensive:
Remember that the pain experience is much different for children than it is for adults. Just because the patient cannot or does not tell you about pain does not mean they aren’t experiencing it. But don’t be intimidated. Using these steps, you can effectively assess and manage your pediatric patients’ pain.
Want to learn more about developing confidence in treating pediatric patients?
Check out Understanding The Pediatric Patient (podcast)
AAP COMMITTEE ON FETUS AND NEWBORN and SECTION ON ANESTHESIOLOGY AND PAIN MEDICINE. Prevention and Management of Procedural Pain in the Neonate: An Update. Pediatrics. 2016;137(2):e20154271
Alexander, J. & Manno, M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann Emerg Med. 2003;41:617-622 Ann Emerg Med. 2003;41:617-622
Campbell, L., DiLorenzo, M., Atkinson, N., & Riddell, R.P. (2017). Systematic Review: A Systematic Review of the Interrelationships Among Children’s Coping Responses, Children’s Coping Outcomes, and Parent Cognitive-Affective, Behavioral, and Contextual Variables in the Needle-Related Procedures Context. Journal of pediatric psychology, 42(6), 611–621. https://doi.org/10.1093/jpepsy/jsx054
Engel G.L. (2012). The need for a new medical model: a challenge for biomedicine. Psychodynamic psychiatry, 40(3), 377–396. https://doi.org/10.1521/pdps.2012.40.3.377
Galinski, M., Picco, N., Hennequin, B., Raphael, V., Ayachi, A., Beruben, A., Lapostolle, F., & Adnet, F. (2011). Out-of-hospital emergency medicine in pediatric patients: prevalence and management of pain. The American journal of emergency medicine, 29(9), 1062–1066. DOI: 10.1016/j.ajem.2010.06.031
IASP Terminology: pain terms https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698
Lerwick J.L. (2016). Minimizing pediatric healthcare-induced anxiety and trauma. World journal of clinical pediatrics, 5(2), 143–150. https://doi.org/10.5409/wjcp.v5.i2.143
McCarthy, A.M., Kleiber, C., Hanrahan, K., Zimmerman, M.B., Westhus, N., & Allen, S. (2010). Factors explaining children’s responses to intravenous needle insertions. Nursing research, 59(6), 407–416. https://doi.org/10.1097/NNR.0b013e3181f80ed5
Principi, T., Schonfeld, D., Weingarten, L., Schneeweiss, S., Rosenfield, D., Ernst, G., Schuh, S., & Scolnik, D. (2018). Update in Pediatric Emergency Medicine: Pediatric Resuscitation, Pediatric Sepsis, Interfacility Transport of the Pediatric Patient, Pain and sedation in the Emergency Department, Pediatric Trauma. Update in Pediatrics, 223–249. https://doi.org/10.1007/978-3-319-58027-2_8
Rutkowska, A., & Skotnicka-Klonowicz, G. Prehospital pain management in children with traumatic injuries. Pediatric Emergency Care Volume 31(5), May 2015, p 317–320 DOI: 10.1097/PEC.0000000000000313
von Baeyer, C.L., Chambers, C.T., Forsyth, S.J., Eisen, S., & Parker, J.A. (2013). Developmental data supporting simplification of self-report pain scales for preschool-age children. The journal of pain, 14(10), 1116–1121. https://doi.org/10.1016/j.jpain.2013.04.008
About the Author
Jonathan Lee is a critical care paramedic with Ornge in Toronto, Canada, with over 25 years of experience in 911, critical care, aeromedical and pediatric critical care transport. Jonathan’s teaching experience includes classroom, clinical and field education as well as curriculum development and design across a number of health professions.
He is currently delivering KinderMedic, a program he developed to improve the confidence and competence of prehospital providers caring for acutely ill children. In addition to his clinical practice, he is also adjunct faculty in the Paramedic Program at Georgian College. Jonathan is a freelance author and has been invited to speak across North America and Europe on topics such as pediatrics, analgesia, and stress.
Jonathan has previously served on committees for professional organizations, including the Ontario Paramedic Association and NAEMT. He is currently pursuing a Master of Science in Critical Care from Cardiff University.
![]()
Community paramedics in Teller County, Colorado, are pioneering new ways to care for mental health patients using cutting-edge technology. Check out what they've learned.

Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management...

For Those Who Love a Good "Oopsie!" At Pulsara, we pride ourselves on enabling secure, HIPAA-compliant communication for healthcare teams. But let’s...

March Recap A New Integration: Improving Data Management, Streamlining Workflows, and Improving Care CoordinationOnly a few days ago, we announced...