In the News: Pulsara's Impact From Preparedness to Lifesaving Care
At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...
4 min read
 Team Pulsara
:
Oct 15, 2021
Team Pulsara
:
Oct 15, 2021

Editor's Note: The following content originally appeared on EMS1.com. Special thanks to our guest blogger, Drew Rinella for EMS1 BrandFocus.
Specialty patients present unique challenges to EMS providers in the field. Whether it's a rare medical condition, an unusual medical device, or an unfamiliar treatment, specialized conditions will require different considerations from more routine calls. But don't worry; even if you aren't familiar with the patient's condition or device, there are some practices you can use to help minimize the degree of unfamiliarity and still provide top-notch care for your patient.
Here are 10 things you need to know about caring for specialty patients and managing resources around their care.
With the ever-increasing cost of health care, home care services are becoming an affordable alternative to residing at a skilled nursing facility. While the cost of private nursing home care has risen at a rate of around 4 percent annually, the cost of in-home care has only risen approximately 1 percent per year. This savings has created an increasingly popular incentive for the disabled and specialty patient to remain at home, increasing their likelihood of needing EMS assistance at some point.
It is impossible to be an expert in every special condition or medical device you will encounter in the field. Patients and their family members, however, are often well versed in the management of the rare medical conditions affecting them. For example, patients receiving Left Ventricular Assist Devices undergo rigorous training in the troubleshooting of their life-saving medical appliance prior to hospital discharge.

In situations where you are unfamiliar with the patient's condition or device, don't hesitate to ask the patient or their family members questions. In many cases, they will likely be able to provide helpful information that can help you get your bearings and provide proper care for the patient.
Online medical control (OLMC) isn’t your only resource for help in unusual situations. Ask your patient if they have been given a hotline number to receive troubleshooting help with their medical device if it malfunctions. If your local protocols permit, utilize this avenue for advice on the most appropriate treatment and transport destination. In some cases, it may even be appropriate to contact the clinical manager of the device manufacturer.
If local protocols permit, consider bypassing the closest facility if it is not equipped to handle your patient. Bariatric beds, pediatricians, and mechanical heart specialists are examples of services that may not be available at smaller hospitals. Initial transport to an inappropriate facility delays the definitive care of your patient and increases overall cost to the patient and their family in the form of bills for redundant hospital exams and ambulance transport flat rates.
Rather than focusing solely on the medical device or chronic condition, consider other causes of the patient’s problem. Just because a patient suffers from a known ailment doesn’t mean a completely unrelated problem can’t pop up acutely. Remember good assessment skills and always be alert to other possible sources of the patient’s problem.

Don’t discount the significant role emotional stress plays in the condition of the specialty patient. For patients who suffer from chronic conditions, their lives are sometimes completely dependent on the proper functioning of a complex medical device, like an LVAD or a defibrillation vest. This can be overwhelmingly stressful, to the point of causing panic attacks. With physical symptoms like shortness of breath and heart palpitations, it can be difficult to tell if the patient is having anxiety, an exacerbation of their medical problem, or both. Management of anxiety should be part of a comprehensive approach to the treatment of these patients.
Try to find out why exactly you were called. Some basic comfort needs can and should be treated without transport. The caregiver of the ground-level-fall hospice patient may simply need some reassurance and help with getting the patient cleaned up and put back into bed. In some states, EMS providers may be called upon to provide symptom control to terminally ill patients in the process of committing physician-assisted suicide, who would similarly not benefit from ambulance transport.
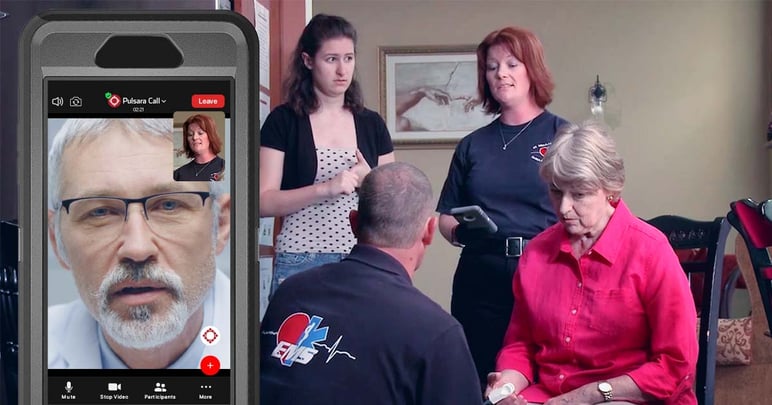
In situations where the moving of a patient could result in unnecessary hazards to field personnel, such as the non-emergency transport of a non-ambulatory bariatric patient to a routine office exam, consider a safer alternative, such as contacting the patient’s physician to inquire if the appointment can be conducted by proxy through on-scene EMS providers. Physical exams can be performed at the direction of the patient’s medical doctor via a live video telehealth encounter, and providers can draw blood and transport the vials to the physician’s office without risking career-ending back injuries.
If your agency utilizes mobile integrated healthcare or community paramedicine, consider referring your specialty patient to MIH personnel. Even if your agency does not have an official MIH program, field providers can still help to prevent unnecessary 911 calls in some cases by visiting specialty patients during times of low call volume.
Encourage your agency’s administrators to evaluate the appropriateness of specialty equipment for your system. Some equipment, such as bariatric ramps, winches, and stretchers, justify their own costs with the first major injury prevented. Agencies should also ensure that providers have access to cellphones or sat phones for contacting emergency hotlines and other resources, in case they need advice on rare specialty patient situations.
Having a plan in place now makes for a smoothly run operation later. This starts with identifying specialized needs within your EMS system and training to meet the need when it arises. Planning now for the inevitable transport of your bariatric shut-in patient can increase operational efficiency and reduce the risk of injury to the providers involved. Quality assurance managers can close the loop by selecting these unusual specialty patient calls for case review, and encouraging the free exchange of ideas for how to handle similar situations in the future.
About the Author
Drew Rinella is the clinical coordinator for Bonner County EMS in rural North Idaho. He is a paramedic, public servant, and competition shooter. Drew is an advocate for quality in EMS and also blogs his crusade against bad EKGs in product advertising.
Editor's Note: This post was originally published in April 2017 and has been updated for accuracy and comprehensiveness.
Pulsara is helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...

December Recap After an incredibly busy events year with 102 conferences, trade shows, and sponsorships, December was on the slower side for us, with...

Editor's Note: In July 2025, EMS1 and Fitch & Associates released their annual EMS trend survey, What Paramedics Want, proudly sponsored by Pulsara....